Rheumatoid arthritis,[1] also called RA, is a chronic autoimmune inflammatory disease. This and osteoarthritis are two of the most common[2] rheumatic and musculoskeletal diseases globally. When a person has RA, their immune system accidentally attacks healthy joints. This results in inflammation, which causes the joints to swell.
RA is typically quite painful for people who live with this condition. It usually involves several[1] joints at once. This not only causes chronic pain but also makes it difficult to maintain balance.
Since RA can be painful and disabling, it’s important to raise awareness of this health condition. Below, find rheumatoid arthritis statistics, as well as information about how this condition is treated.
Rheumatoid Arthritis Facts
- In the U.S., 21.2%[3] of the adult population has some form of arthritis, which could include rheumatoid arthritis.
- Arthritis is more common in women, who have a prevalence of 24.2%,[3] compared to 17.9%[3] of men.
- In the United States, an estimated 0.6% to 1.0%[4] of adults have rheumatoid arthritis specifically. -The mortality rate is 1.59 times[5] higher in patients with rheumatoid arthritis compared to those without.
Rheumatoid Arthritis Statistics In The United States
Prevalence Of Arthritis In The United States
- Rheumatoid arthritis is just one type of arthritis. According to data from the National Health Interview Survey, 53.2 million[3] U.S. adults have any type of arthritis. This is equal to 21.2%[3] of the adult population.
- Remember that this figure includes any type of doctor-diagnosed arthritis. So, it includes not only rheumatoid arthritis but also gout, lupus, fibromyalgia, or any other type of arthritis.
- Data from the U.S. shows that 1.3 million adults,[4] or 0.6% to 1.0%[4] of the population, have rheumatoid arthritis.
Prevalence Of Arthritis By Sex
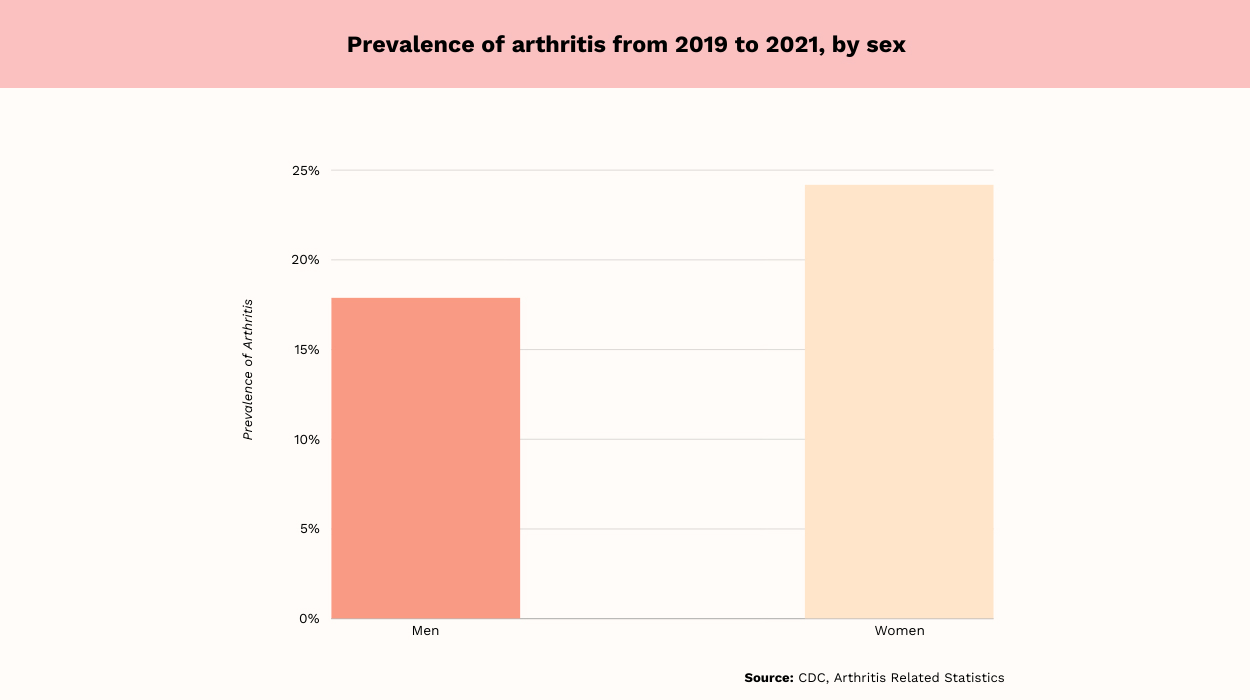
- According to the National Health Interview Study, or NHIS, doctor-diagnosed arthritis is more common in women than men. From 2019 to 2021, prevalence was 24.2%[3] in women and 17.9%[3] in men.
Per Dr. Praveen Guntipalli, M.D., Double Board Certified in Internal Medicine and Obesity Medicine, hormones explain the fact that rheumatoid arthritis prevalence is higher in women compared to men. She says, “Estrogen, in particular, is believed to influence immune system functioning, potentially triggering autoimmune responses.” She further states, “Genetic predispositions and environmental factors like smoking are also contributing factors to this gender disparity.”
Prevalence Of Arthritis By Race/Ethnicity
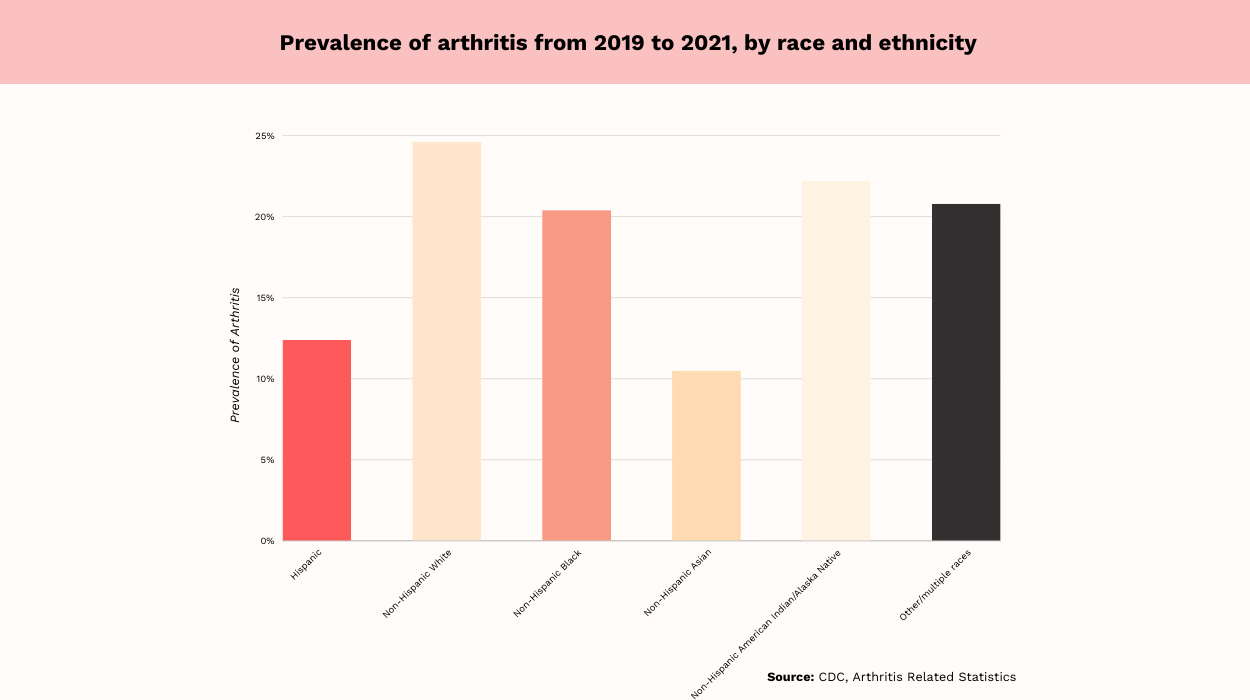
During 2019 -2021, arthritis prevalence varied by race and ethnicity, according to the results of the NHIS. Below are the doctor-diagnosed prevalences based on race and ethnicity:
- 12.4%[3] prevalence among Hispanic adults, equal to 5.2 million[3] people.
- 24.6%[3] prevalence in non-Hispanic White adults, equal to 39.1 million[3] people.
- 20.4%[3] prevalence in non-Hispanic Black adults, equal to 6.0 million[3] people.
- 10.5%[3] prevalence in non-Hispanic Asians and other Pacific Islander adults, equal to 1.6 million[3] people.
- 22.2%[3] prevalence in non-Hispanic American Indian or Alaskan Native adults, equal to 0.4 million[3] people.
- 20.8%[3] prevalence in adults of other or multiple races, equal to 1.0 million[3] people.
As Dr. Guntipalli explains, “The higher prevalence of RA in certain racial and ethnic groups can be attributed to a complex interplay of genetic predispositions and environmental factors.” She further states, “Socioeconomic disparities, which influence access to healthcare and health literacy, also significantly impact the prevalence and management outcomes in these populations.”
Prevalence Of Arthritis By Age
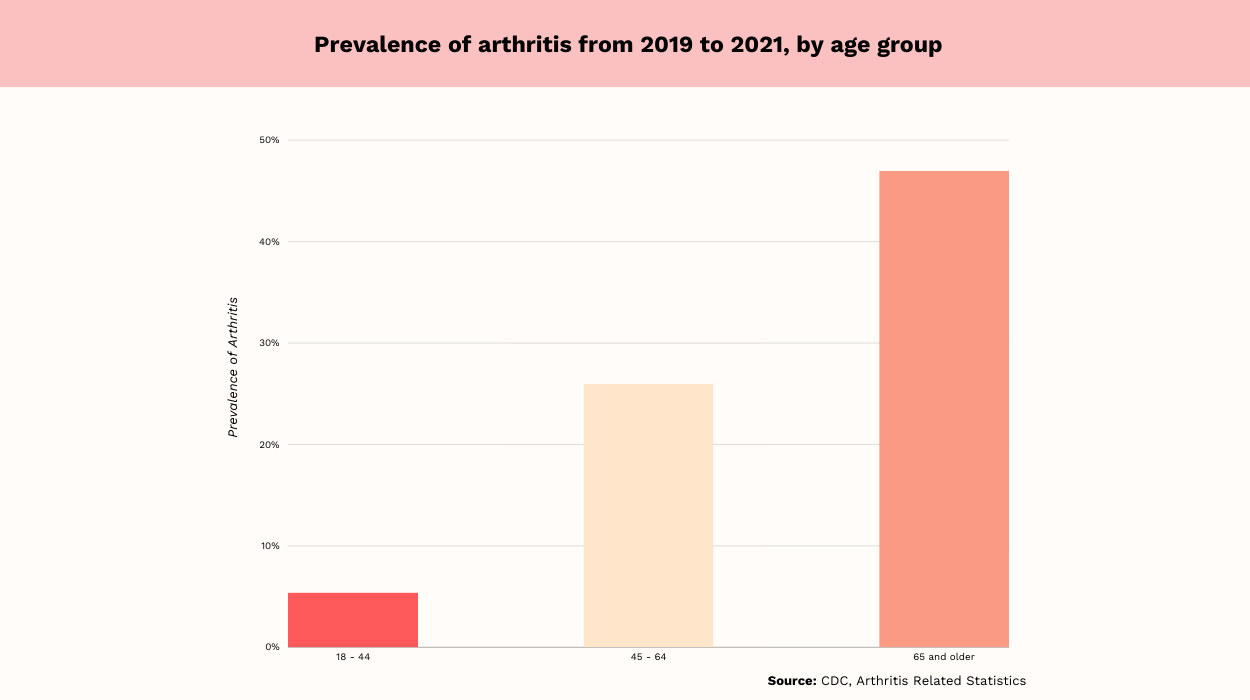
According to the 2019-2021 NHIS, the prevalence of arthritis varied as follows according to age:
The data shows that arthritis prevalence increases with age. Just over five[3] out of 100 adults aged 18 to 44 have arthritis. This is compared to almost half[3] of those 65 and older.
Steven Fiore, MD, Board-Certified Orthopedic Surgeon, states, “While rheumatoid arthritis can develop at any age, the risk may indeed increase with age.” He further states, “Aging is associated with changes in the immune system and joint structures, making older individuals more susceptible to inflammatory conditions like rheumatoid arthritis.”
It is no surprise, then, that arthritis rates are highest among those aged 65 and older.
Rheumatoid Arthritis Facts To Know
There are some additional facts to know related to rheumatoid arthritis, including global prevalence. According to global data, the incidence of rheumatoid arthritis varies by country.
Consider the facts below on global rheumatoid arthritis incidence:
- Ireland has the largest global incidence of RA, at 30.03[6] cases per 100,000 people.
- Finland has the second highest incidence rate globally, at 27.89[6] per 100,000 people.
- Kazakhstan, in central Asia, has the third highest RA incidence rate, at 25.5[6] per 100,000 people.
- The incidence of RA increased in most countries[6] across the globe between 1990 and 2019, with an estimated annual percent change of .37%.
Another important factor to consider when evaluating the global burden of arthritis is the rate of disability-adjusted life years. As of 2017, the age-standardized rheumatoid arthritis DALYs were 43.3[7] per 100,000 people in the global population.
Finally, rheumatoid arthritis isn’t a health condition limited to the United States. Across the globe, 18 million people[8] live with rheumatoid arthritis.
Overweight/Obesity And Arthritis
Rheumatoid arthritis is linked to overweight and obesity. Some studies have shown mixed results, but obesity does seem to moderately increase[9] the risk of developing RA.
In addition, rheumatoid arthritis severity may be higher among those who are obese. For example, research shows[9] that individuals with obesity are less likely to respond positively to medication.
On the other hand, individuals with obesity tend to have better long-term outcomes with rheumatoid arthritis. They are less likely[9] to die, which may be because poor disease management can lead to weight loss. People with lower BMI may lose weight due to poor health, explaining the link between obesity and reduced death risk.
Severe Joint Pain And Arthritis
Joint inflammation from conditions like rheumatoid arthritis can be quite painful. According to 2017 data from the United States, the prevalence[10] of severe pain with arthritis is as follows:
- 36.0%[10] in women, compared to 27.3%[10] in men
- 35.6%[10] in adults aged 45 to 64, compared to 33.0%[10] in those 18 to 44 and 25.1%[10] in those 65 and older
- 50.9%[10] in non-Hispanic Blacks compared to 42.0%[10] in both Hispanics and American Indian/Alaskan Natives
- 37.4%[10] in those of other or multiple races, and 27.7%[10] in Asians, and 27.4%[10] in non-Hispanic Whites
- 37.2%[10] in obese adults, compared to 28.6%[10] in overweight adults and 29.1%[10] in underweight adults
The data shows that women are more likely[10] than men to experience severe joint pain from arthritis. Obese adults are more likely[10] than both overweight and underweight adults to experience severe joint pain. Finally, non-Hispanic Blacks are most likely[10] to experience severe joint pain; non-Hispanic Whites are least likely.
Disability/Limitations And Arthritis
Having an autoimmune disease like rheumatoid arthritis can be quite debilitating. The government collects and reports data on disability and limitations from arthritis, which shows the negative impact of arthritis.
According to the most recent data, 36.7%[11] of men and 46.8%[11] of women with arthritis experience activity limitation. For women, the highest prevalence of activity limitation from arthritis was in Oklahoma, at 56.9%.[11] For men, Tennessee had the highest prevalence of activity limitation from arthritis, at 53.7%.[11]
The lowest prevalence of activity limitation from arthritis was in Wyoming for both men and women. In that state, the prevalence of activity limitation was 30.8%[11] for women and 25.8%[11] for men.
Common difficult activities for individuals with arthritis include:[12]
- Firmly holding small objects.
- Reaching overhead.
- Sitting for around two hours.
- Lifting or carrying 10 pounds.
- Climbing an entire flight of stairs without stopping.
- Pushing or pulling heavy objects.
- Walking for one-fourth of a mile.
- Standing for around two hours.
- Completing activities such as stooping, bending, or kneeling.
Arthritis Costs
The burden of disease from arthritis can be quite costly. The most recent data from 2013 show that arthritis costs the United States $140 billion[13] annually in medical expenses. This is equal to an extra $2,117[13] per person with arthritis.
Lost wages from arthritis cost the United States $164 billion[13] annually in 2013. This is equal to $4,040[13] per person with arthritis.
Some types of arthritis are more costly than others. Osteoarthritis, the most common type, cost the U.S. $16.5 billion[13] per year in hospitalization expenses alone in 2013. A 2018 meta-analysis found that rheumatoid arthritis costs $12,509[14] in direct medical expenses per patient per year.
The global burden of disease from arthritis is also high. In Japan, lost productivity from rheumatoid arthritis alone costs $9.80 billion[15] per year. In Mexico, the costs of inpatient treatment for RA totaled $8.9 million[16] in 2017.
Rheumatoid Arthritis Symptoms
When a person has rheumatoid arthritis, they will experience flares, during which they have symptoms of the disorder. At other times, they will be in remission.
When a person has symptoms related to RA, they will experience the following:[1]
- Aches or pains in several joints.
- Joint stiffness in multiple joints.
- Swelling and tenderness in several joints.
- Weight loss.
- Feelings of fatigue.
- Weakness.
- Fever.
- Symptoms that occur on both sides of the body, such as in both hands.
Risk Factors
Some people are at greater risk of RA than others. When people develop rheumatoid arthritis, it is usually because of a combination of genetics and environmental risk factors.
The following risk factors[1] are known to increase the chances of developing rheumatoid arthritis:
- Older age.
- Being female compared to male.
- Having a certain genotype.
- Smoking.
- Never giving birth as a woman.
- Growing up in a low-income household.
- Exposure to cigarette smoke as a child.
- Obesity.
One risk factors study found[17] that the greatest risk factors for RA include female sex, tobacco smoke exposure, family history, and genetics. Smoking risk attribution, in addition to gender and genetics, appears to be high.
While a risk factor increases the chances that a person will develop inflammatory arthritis, protective factors reduce the risk. One protective factor identified for RA is breastfeeding.[1] Women who have breastfed a baby are at lower risk of rheumatoid arthritis.
Rheumatoid Arthritis Treatments
Rheumatoid arthritis is a chronic disease, but it can be managed with medication and lifestyle changes. These are described in more detail below.
Medication For RA
The first choice of medication for treating RA is a class of drugs called disease-modifying antirheumatic drugs. These medications slow disease progression[1] and stop the joints from becoming deformed.
Another choice of medications for treating RA is called biologicals. These medications include[18] etanercept and adalimumab. Medications in this class can reduce inflammation but have side effects.
Nonsteroidal anti-inflammatory drugs may also be used to reduce[19] pain and swelling. Medications in this class include naproxen and celecoxib. Naproxin was found to be the most effective, while celecoxib had fewer side effects.
Finally, cortisone, a hormone with anti-inflammatory properties, may be used.
Lifestyle Changes For RA
Rheumatoid arthritis can also be managed[20] with these strategies:
- Avoid injury to the joints by limiting repetitive motions.
- Participate in regular moderate-intensity physical activity, such as walking.
- Take an arthritis management class to learn strategies for living with the disease.
- See a doctor for an early diagnosis as soon as symptoms appear.
- Lose weight, which can improve[21] disease activity.
Expert Insights
When learning about RA treatment, it’s helpful to turn to expert medical advice. According to Dr. Guntipalli, the treatment of RA requires a holistic approach that encompasses both medical and lifestyle interventions.
“This includes tailored medication regimens, often involving DMARDs and biologics to control inflammation and prevent joint damage,” she says. Dr. Guntipalli goes on to say, “Equally
important are lifestyle modifications like regular physical activity, especially exercises that strengthen muscles without putting undue stress on joints, and a balanced diet rich in anti-inflammatory foods.”
DMARDs stand for disease-modifying anti-rheumatic drugs and may be used in the treatment of RA.
Research[22] does confirm that an anti-inflammatory diet can be beneficial for reducing subjective pain in RA patients. The Mediterranean diet, as well as vegetarian and vegan diets, may be beneficial. The Mediterranean diet emphasizes[23] anti-inflammatory foods, including fruits, vegetables, and olive oil.
Taylor Wilson, Founder of Active Recovery Companion and Certified Recovery and Health Specialist, agrees that dietary interventions are critical for RA management. She says, “Maintaining a healthy and balanced diet can help reduce inflammation and manage symptoms. Foods high in omega-3 fatty acids, antioxidants, and fiber are especially beneficial.”
Wilson further states, “Low-impact exercises like swimming, walking, or yoga can help improve joint flexibility, reduce pain, and increase overall well-being.”
Dr. Fiore agrees with the other medical opinions given here. “To improve the quality of life with rheumatoid arthritis, patients can engage in regular low-impact exercises, maintain a healthy weight, and work closely with a healthcare team to manage symptoms through medications and lifestyle modifications,” he says.
Conclusion
Rheumatoid arthritis is an inflammatory arthritis condition that can cause joint swelling and pain. It affects 0.6% to 1.0%[4] of adults in the United States. So, it makes up just a portion of the 21.2%[3] of adults with arthritis.
RA can be quite painful and disabling, but with treatment, the condition can be managed. If you or someone you love has RA, seeing a doctor is important.
Frequently Asked Questions
Rheumatoid arthritis mortality data show the mortality rate is 1.59 times[5] higher in those with RA. However, you can live a long life by treating the condition and managing comorbidities[5] like heart disease.
Medication is considered essential[20] for treating rheumatoid arthritis. It can slow disease progression and even lead to remission. Without medication, RA is likely to progress more quickly.
In the United States, just 0.6% to 1.0%[4] of adults have rheumatoid arthritis. So, the chances of developing RA are quite low.
Rheumatoid arthritis can cause severe pain and disability, but it is treatable. Treatment can improve quality of life.
 Evidence Based
Evidence Based
