A migraine[1] is a type of headache that causes repeated attacks. During migraine attacks, a person experiences moderate to severe pulsating or throbbing. This occurs on just one side of the head.
Migraines can be quite debilitating, causing people to seek medical care or take brain-boosting supplements for relief. Migraine statistics provide insights into how many people experience this condition. Below, find the most recent facts and figures about migraine attacks.
Key Facts About Migraine Rate In The USA
In 2021, 4.3%[2] of U.S. adults said they’d been bothered a lot by a migraine or headache over the last three months.
Among women, 6.2%[2] had been bothered by migraine or headaches in the last three months.
Among men, 2.2%[2] were bothered a lot by migraine or headaches over the last three months.
In women aged 18-44, 7.4%[2] were bothered a lot by a migraine or headache over the last three months.
Key Migraine Facts
- In 2021, 4.3%[2] of U.S. adults said they’d been bothered a lot by a migraine or headache over the last three months.
- Among women, 6.2%[2] had been bothered by migraine or headache in the last three months.
- Among men, 2.2%[2] were bothered a lot by migraine or headaches over the last three months.
- The highest rates of being bothered by migraines or headaches were in women aged 18-44. In this group, 7.4%[2] experienced a migraine or headache that greatly bothered them over the last three months.
Migraine Statistics
Migraine Statistics By Sex And Age Group
- In women aged 18-44, 7.4%[2] have experienced headaches or bad migraines that bother them a lot. Among men the same age, 2.5%[2] experienced migraine or headache.
- In women ages 45-64, 6.7%[2] have experienced a headache or bad migraine that bothers them a lot. This is compared to 2.4%[2] of men the same age.
- In women aged 65 and older, 3.1%[2] have been bothered a lot by a migraine or headache. In men this age, 1.5%[2] have experienced a headache or migraine that bothered them a lot.
These data indicate the percentage of people who were bothered a lot by headaches or migraine over the last three months. They are up-to-date as of 2021.
There are confirmed sex-related differences in migraine prevalence. Women in all age groups are more likely than men to have been bothered a lot by headaches or migraine.
Younger adults aged 18-44 are more likely to experience headaches or migraines. Adults 65 and older are least likely to experience them.
According to Dr. Kevin Huffman,[3] Doctor of Osteopathic Medicine and board-certified bariatric physician, hormones play a role in increased migraine risk among women. He says, “Although shifts in estrogen are typically associated with the menstrual cycle and thought to trigger migraine in many women, the hormonal basis for the disorder is bolstered by evidence that some women first experience these excruciating headaches around puberty and then see their migraine patterns shift through pregnancy and into menopause.”
Dr. Laurel Steinberg, Ph.D., a migraine prevention expert, agrees. She says, “Women experience dramatic hormone shifts throughout the month, which can contribute to the migraine trigger load.”
Migraine Statistics By Race And Ethnicity
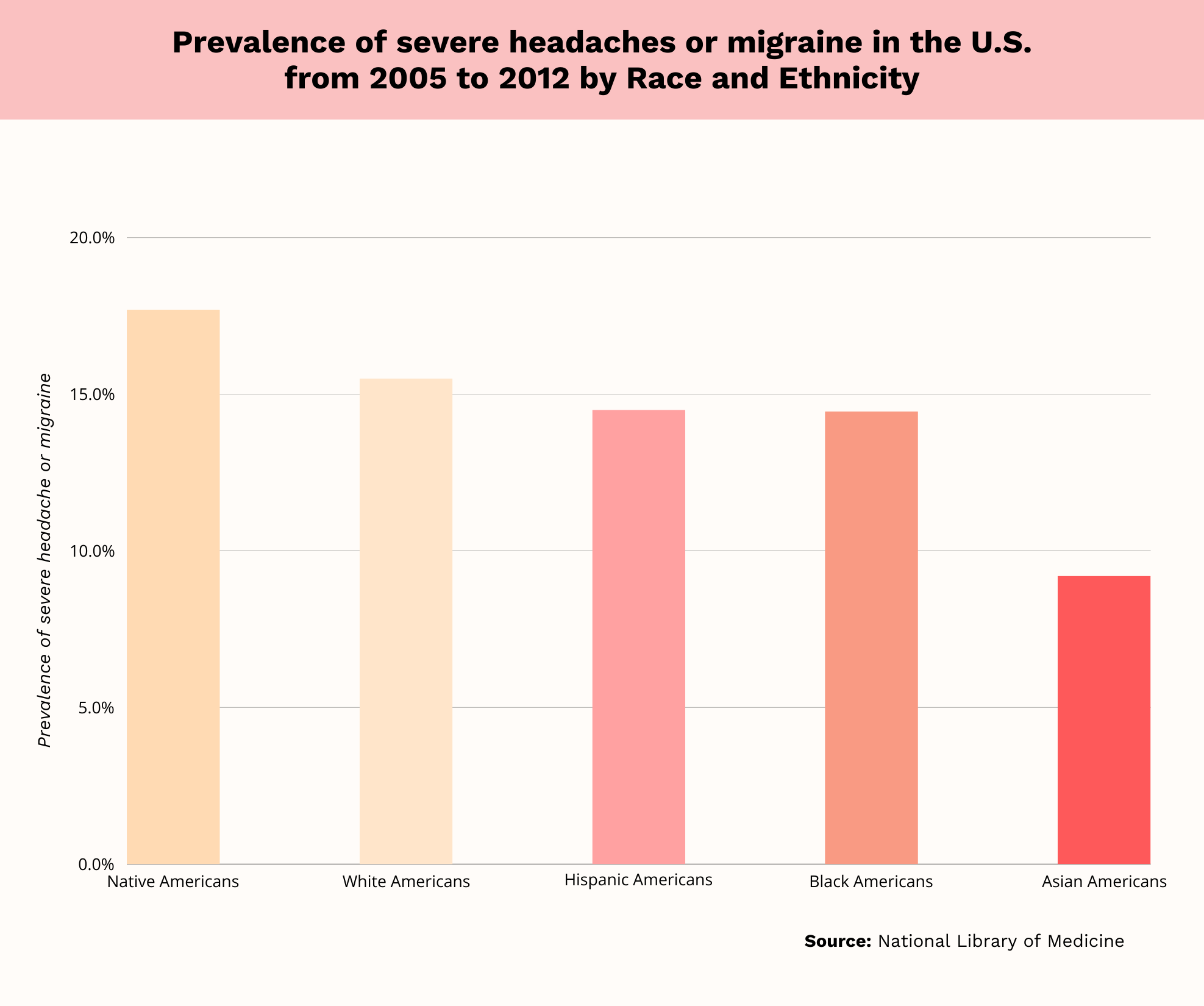
- Native Americans have the highest rates of severe headaches or migraine, at 17.7%.[4]
- Among Whites, 15.5%[4] experience severe headaches or migraines.
- In Hispanics, 14.5%[4] experience severe headaches or migraines.
- The rate of severe headache or migraine is 14.45%[4] in Blacks.
- Among Asians, 9.2%[4] experience severe headaches or migraines.
These data are from the 2005-2012 National Health Interview Survey, which provides the most recent statistics. According to this national survey, there is racial/ethnic variation in migraine prevalence.
Native Americans have the highest rates of severe headaches and migraines among all groups. They are closely followed by Whites. Asians have the lowest prevalence of severe headaches and migraines among all groups.
According to Dr. Huffman, there are several causes of racial and ethnic variation in migraine prevalence. He states, “As an osteopathic physician who has worked for years with patients with migraine, I’ve witnessed and been inspired by the intricate role that the multitude of factors plays in a higher prevalence of migraine in certain racial and ethnic groups.”
He adds, “There are genes for migraines that play a role, but only if they exist more directly across a community.” Finally, he states, “Social determinants, including aspects of healthcare access; socioeconomic status; education levels; and numerous environmental aspects all play a role.”
Beliefs About Causes Of Migraine
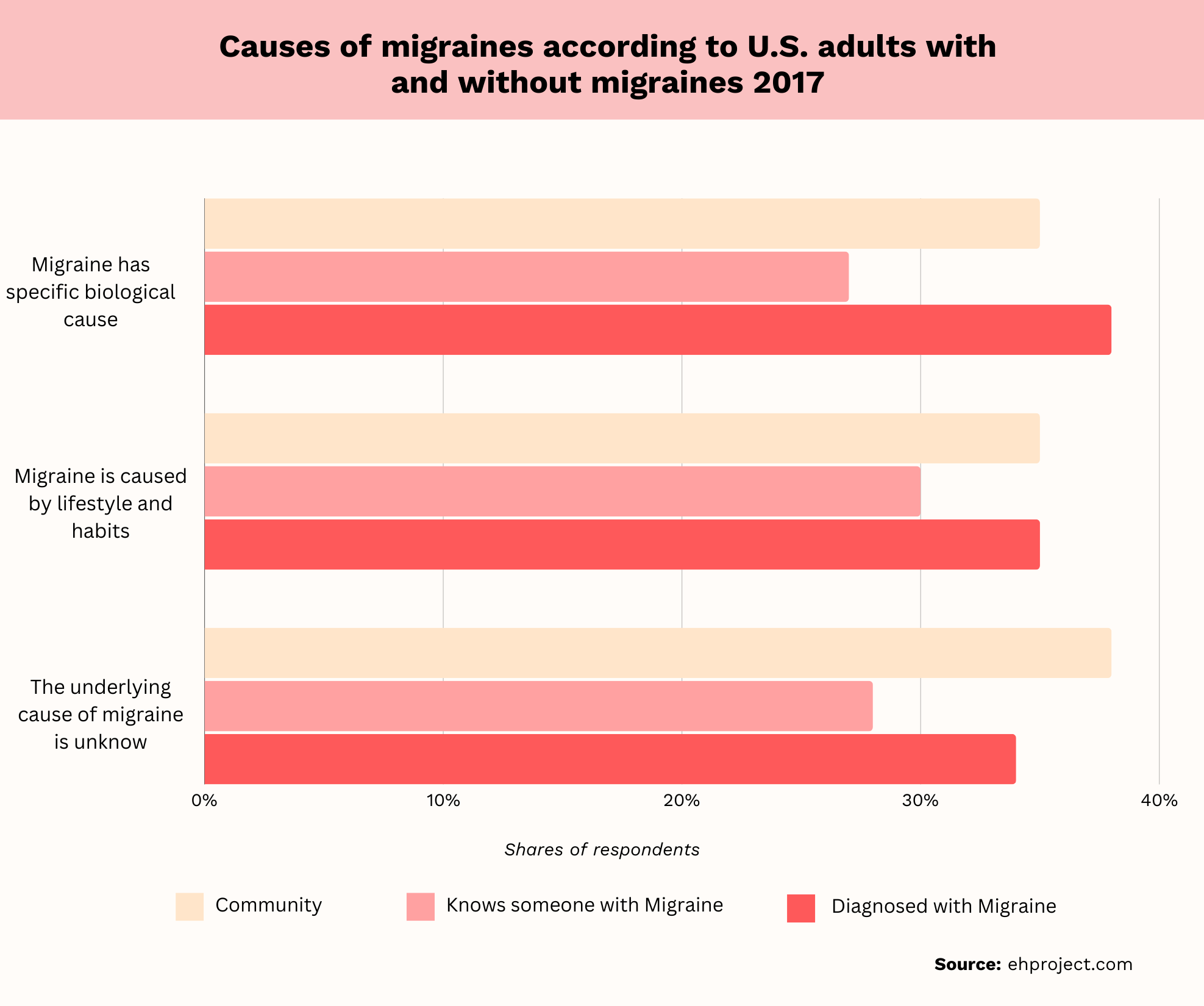
- In people diagnosed with migraines, 38%[5] believe there are specific biological causes.
- In addition, 28%[5] of people diagnosed with migraines believe lifestyle and habits are the cause.
- Finally, 34%[5] of people with migraines believe the cause is unknown.
The most common cause of migraines, according to those diagnosed with them, is biological factors. A significant portion of people, just over one-third,[5] believe the cause is unknown. Just over one-fourth[5] of people with migraines believe lifestyle and habits are to blame.
Migraine Facts To Know
There are additional migraine headache statistics beyond the general prevalence data reported above. Find some more interesting facts about headache disorders below.
Migraines Are A Global Health Problem
Headache disorders don’t just affect Americans; they are a global health concern. As of 2019, there were 581,761,847[6] global migraine cases, according to a global burden of disease study. This represented a 16%[6] increase in migraines since 1990.
High socioeconomic status countries had the highest migraine prevalence, at 22,606[6] cases per 100,000 people. Finally, women and those aged 30-39[6] were most likely to be affected by migraine headaches.
There Are Other Headache Disorders Aside From Migraines
Chronic migraines are just one of the headache disorders. Tension-type headaches are also common.
In 2019, there were 964,808,567[6] cases of tension-type headaches across the globe. This was a 37%[6] increase since 1990.
There Are Differences Between Chronic And Episodic Migraines
Some people with headache disorders experience chronic migraines. Others experience episodic migraines, meaning they have a migraine attack less often.
For a chronic migraine diagnosis, a person must have 15 headaches monthly[7] for at least three months. People with chronic migraines experience migraine symptoms less frequently. They have about one or two migraine attacks each month.
Chronic migraines are less common than episodic migraine symptoms. Just 1%-2%[8] of the general population and 8%[8] of people with migraines experience chronic migraine symptoms.
In most cases, chronic migraines develop from episodic migraines. Risk factors[8] for conversion to chronic migraine are numerous. They include obesity, depression, stressful life events, overuse of acute migraine medications, and ineffective treatment.
Chronic Migraines Are Linked To Poor Mental Health
Chronic migraine statistics show people who have chronic migraine headaches are at risk of poor mental health. One study found 56.6%[9] of people with chronic migraines had depression. This was compared to 30.0%[9] of those with episodic migraines.
Furthermore, 48.4%[9] of people with chronic migraines had anxiety, compared to 28.1%[9] of those with episodic migraines. Having depression increased the risk of moderate to severe disability from migraines by 56.0%.[9] Having anxiety increased the risk by 39.0%.[9]
Chronic Migraines Are Costly To Treat
There is a high economic burden associated with chronic migraine. One study found that progression[10] from episodic migraine to chronic migraine was associated with significant costs.
In the study, people who progressed to chronic migraine incurred $1,790[10] in monthly costs, on average. Before progression, the monthly cost for migraine treatment was $1,414[10] per person.
Symptoms Of A Migraine
When people have migraines, they experience repeated migraine attacks. The most common symptoms[1] during an attack are moderate to severe pulsating and throbbing. This pain occurs on one side of the head.
Other migraine symptoms include:
- Elevated sensitivity to lights, smells, and sounds.
- Nausea.
- Vomiting.
- Increased pain with movement, exercise, or coughing/sneezing.
Beyond these classic symptoms, some people may experience migraine with aura. This type of migraine involves visual and neurological disturbances before the headache. These symptoms typically last a maximum of one hour and include:[1]
- Vision loss.
- Difficulty speaking.
- Numbness or muscle weakness on one side of the body.
- Confusion.
- Tingling in the hands or face.
Most people experience migraines without aura, also called common migraines. After a migraine, people may feel exhausted or confused.
Migraine Causes
There are several triggers and risk factors for migraines. However, the physiological cause[1] is the activation of nerve fibers. These nerve fibers are found in the wall of brain blood vessels inside the meninges.
The meninges are membrane layers[1] that protect the brain and spinal cord. When nerve fibers traveling inside the meninges are activated, a migraine results.
According to Dr. Walker Porterfield, lead chiropractor at Clarity Chiropractic, “There are several causes of migraines that I see; the biggest one is dural tension, which can affect blood flow to the brain.” He further explains, “The dura is essentially a protective loose sack that surrounds the brain and spinal cord; when that dura gets pulled in one direction, it can drastically alter blood supply, leading to a piercing migraine.”
Dr. Steinberg offers a slightly different perspective, stating, “The mechanism of migraine is turned on when the daily trigger load, or all of the activating events that stimulate migraine, cumulatively rises to a point above the migraine threshold.” She adds, “Some of the activating events that contribute to the migraine trigger load include, but are not limited to, diet, hormonal fluctuations in women, barometric pressure, how we relate to stress, sleep disturbances, and the side effects of various medications.”
Migraine Risk Factors
There are multiple risk factors that increase the likelihood that someone will experience a migraine. These include:[1]
- Changes to the weather or environment that come on suddenly.
- Lack of sleep or too much sleep.
- Strong odors.
- Stress.
- Strong emotions.
- Over exerting oneself.
- Sudden or loud noises.
- Motion sickness.
- Low blood glucose levels.
- Skipping meals.
- Tobacco use.
- Mood disorders, including major depression.
- Anxiety.
- Trauma to the head.
- Being hungover.
- Certain medications.
- Hormonal fluctuations.
- Exposure to bright or flashing lights.
There are a variety of factors that increase the risk of migraine attacks. These factors can vary among different migraine sufferers. What is a risk factor for one person may not affect another.
For those with migraines, it’s important to identify triggering factors and learn how to avoid them, if possible.
Genetic Risk Factors
Some people may have a genetic predisposition to migraines. Numerous gene variants[11] have been found to lead to small increases in overall migraine risk. There are also genes that contribute to both migraine and comorbid conditions like major depression.
Consequences Of Migraine
Unfortunately, untreated or poorly managed migraines affect quality of life negatively. One study assessed the quality of life in people with both episodic migraines and chronic migraines. Results revealed the following:
- In 16.8%[12] of those not in a relationship at the time of the study, headaches had caused relationship problems.
- Among those in a relationship but not living together, 17.8%[12] said migraines affect their relationship negatively.
- Among people answering questions about careers and finances, 32.7%[12] stated headaches negatively affected their careers.
- Finally, 32.1%[12] of people stated they worried about their financial security because of migraines.
How To Treat Migraine
There are two overarching types of migraine treatments: Preventive and acute.[1] In the short term, the goal of treatment is to alleviate symptoms. Some short-term treatments include drinking water, placing ice over the forehead, and resting in a quiet, dark room.
Medications For Migraine Treatment
Aside from taking the steps above, people may take medications for acute migraine treatment. The following drugs may be used to treat acute episodic migraine:
- Triptans.
- Ergot derivatives.
- Non-prescribed pain relievers like ibuprofen, aspirin, and acetaminophen for mild migraines.
- Nausea relief drugs.
- Combination drugs containing acetaminophen plus caffeine.
- Narcotic drugs, which should never be used for chronic migraines.
A doctor will work with you to decide which medication is the best choice for the acute treatment of migraines. You may have to try several options before you find the best fit for you.
There are also medications that can prevent migraines. Some common medications[1] for episodic migraine prevention include enenmab and galcanezumab-gnlm. These prophylactic medications are taken daily to reduce the occurrence of migraine attacks.
Natural Migraine Treatments
Finally, some people may choose natural migraine treatments.[1] This involves taking supplements, including riboflavin, magnesium, and coenzyme Q10. Some people may use butterbur, which is a medicinal plant.
Biofeedback and relaxation training can also be beneficial for treating migraines.[1] These methods can reduce pain and help people cope with migraine symptoms.
Transcranial Magnetic Stimulation
When people do not respond to migraine medications, they may benefit from transcranial magnetic stimulation or TMS. This procedure uses a device placed against the forehead to stimulate specific brain regions.
A systematic review of eight different studies found TMS is beneficial for treating migraines.[13] Analysis of the studies in the review showed TMS reduces pain and frequency of headaches in those with chronic migraine. On average, TMS reduced migraine frequency by about 8 days[13] per month.
Preventive Measures
Certain lifestyle factors can prevent migraines.[1] For instance, getting regular exercise can prevent migraines. Some people may find that certain foods trigger migraine attacks, so avoiding these can be helpful.
It’s also important to consume enough water[1] and eat regular meals. A consistent sleep schedule can also be beneficial. Finally, since obesity increases migraine risk, weight loss may be helpful.
Dr. Jason Winkleman, a naturopathic doctor and chiropractor specializing in chronic pain, states, “The best thing people can do to prevent migraines is to avoid their triggers and correct their determinants of health.” He adds, “Migraine sufferers need to spend a lot of time logging their migraines and making correlations to everything else going on in their lives.” Finally, he says, “Once this is more understood, you have to come up with a plan to make sure that you are eating right and consistently, getting the right amount of sleep, and staying active after a stressful event to prevent your cortisol levels from crashing too quickly.”
Dr. Huffman agrees, stating, “I am always conscious to advise about the obvious lifestyle tactics towards the prevention of migraines – physical conditioning through regular exercise, maintaining a balanced diet, proper hydration, and getting sufficient hours of healthy sleep.”
Conclusion
Migraines can be quite debilitating,[2] and they affect more women[2] than men. Fortunately, there are treatments available to alleviate migraines. This can include pharmacologic treatment, lifestyle modifications, and natural remedies.
If you experience chronic migraines, you are not alone. A headache specialist can help you identify the cause and develop a treatment plan that meets your nee
Frequently Asked Questions
To be diagnosed with chronic migraine,[7] a person must have at least 15 headaches monthly for at least three months. Eight of these headaches must be migraines. Episodic migraine involves about one to two migraines a month.
Research[2] shows that women and people ages 18-44 are most likely to experience migraine headaches.
There is not one single cause of migraine headaches. Rather, several risk factors increase the chances of having migraines. Genetics,[1] medical conditions, psychiatric diagnoses, and sleep disorders are some risk factors for migraines.
 Evidence Based
Evidence Based
