Most of us know that good sleep is important for health. However, it can be difficult to get enough rest each night.
Busy schedules can push bedtime later; Early morning wake-up calls can cut into sleep time. For some people, sleep is elusive, and falling and staying asleep can seem impossible.
Insomnia[1] is diagnosed when people constantly struggle to fall or stay asleep, or they have poor quality sleep. If you cannot fall asleep or you wake frequently at night, you may have insomnia.
It turns out that this is a relatively common problem. Below, learn some of the top insomnia statistics. These data indicate how prevalent insomnia is, as well as who it’s most likely to affect.
Key Facts About Insomnia Rate In The USA
In 2020, 14.5%[2] of U.S. adults had trouble falling asleep all or most days within the previous 30 days.
Non-Hispanic Whites are the most likely to report sleep difficulties, with 21.0%[2] struggling to stay asleep most days.
Among women, 17.1%[2] struggled to fall asleep all or most days within the last month in 2020.
In men, 11.7%[2] struggled to fall asleep all or most days within the last month in 2020.
Key Insomnia Facts
- In 2020, 14.5%[2] of U.S. adults had trouble falling asleep all or most days within the previous 30 days.
- Non-Hispanic Whites are the most likely to report sleep difficulties, with 21.0%[2] struggling to stay asleep most days.
- Among Blacks, 15.4%[2] struggle to stay asleep all or most days, compared to 10.6%[2] of Hispanics.
- Among women, 17.1%[2] struggled to fall asleep all or most days within the last month in 2020.
- In men, 11.7%[2] struggled to fall asleep all or most days within the last month in 2020.
Insomnia Statistics
Insomnia Statistics By Age
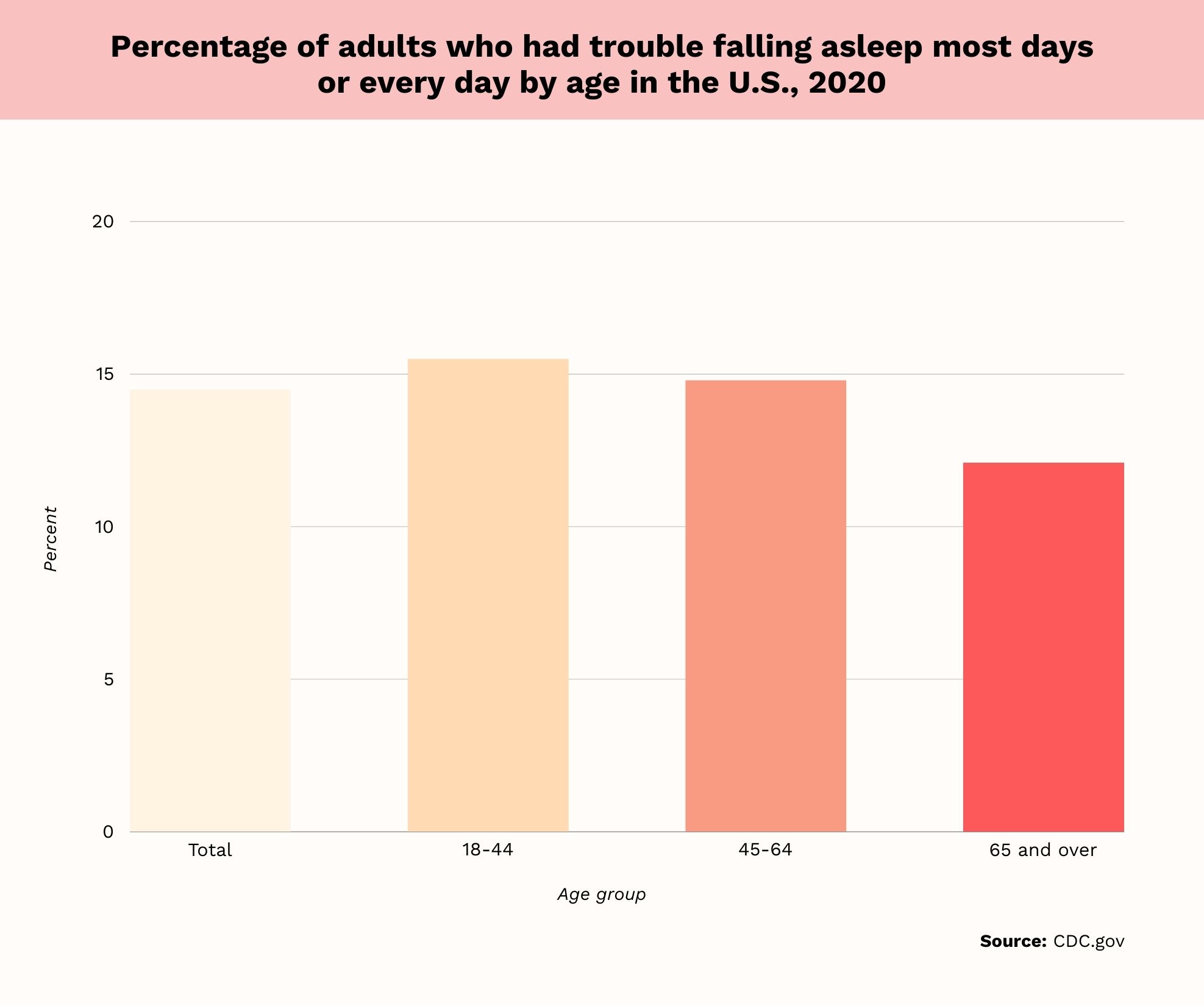
- In 2020, 14.5%[2] of U.S. adults reported trouble falling asleep all or most days over the last month.
- Among those aged 18 to 44, 15.5%[2] had trouble falling asleep all or most days.
- Of those aged 45 to 64, 14.8%[2] struggled to fall asleep, compared to 12.1%[2] of 65 and older.
Sleep difficulties are more common among younger adults, with problems related to falling asleep declining with age. Those aged 18-44 have the highest prevalence of trouble falling asleep. Those aged 65 and older have the lowest prevalence of struggling to fall asleep.
Insomnia Statistics By Sex
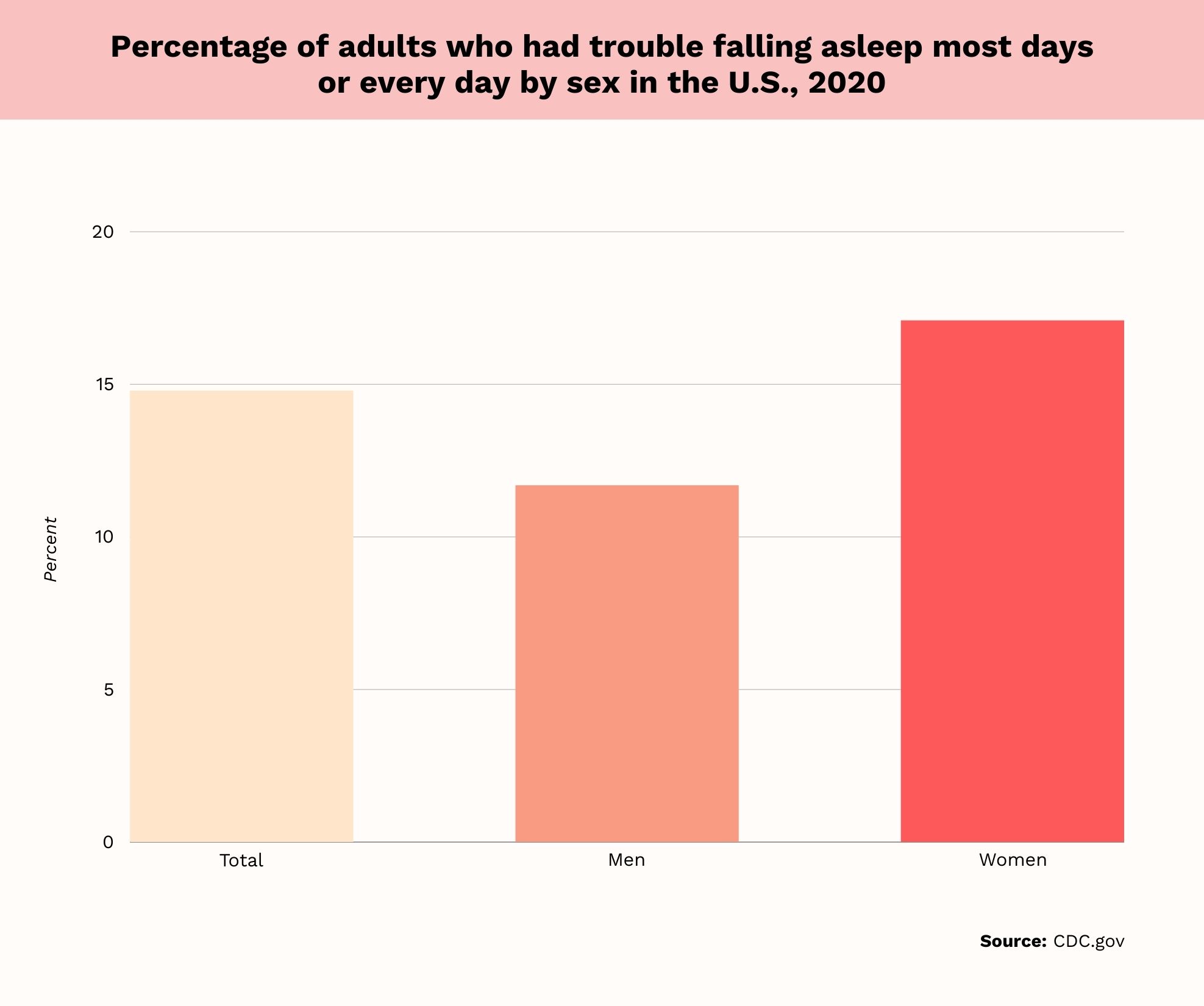
- As of 2020, 17.1%[2] of women said they had trouble falling asleep all or most nights within the last month.
- In the same year, 11.7%[2] of men had trouble falling asleep all or most nights.
More women than men have a hard time falling asleep all or most nights. The same gender disparity exists when evaluating the proportion of people who have difficulty staying asleep. In 2020, 20.7%[2] of women had difficulty staying asleep all or most days within the past month. Among men, 14.7%[2] had difficulty staying asleep all or most days.
“Women are more susceptible to insomnia than men, partly due to hormonal fluctuations during the menstrual cycle, pregnancy, and menopause,” says Marissa Moore, Licensed Professional Counselor, Therapist, MA, LPC, and Mental Health Consultant writer at Mentalyc.
Bijoy E. John, MD, board-certified physician and practicing sleep specialist, says, “Insomnia is up to two times more common in women than in men.” He further states, “There are quite a few factors at play, such as hormonal changes, menopause, mood disorders, and pregnancy, to name just a few.”
Insomnia Statistics By Race And Ethnicity
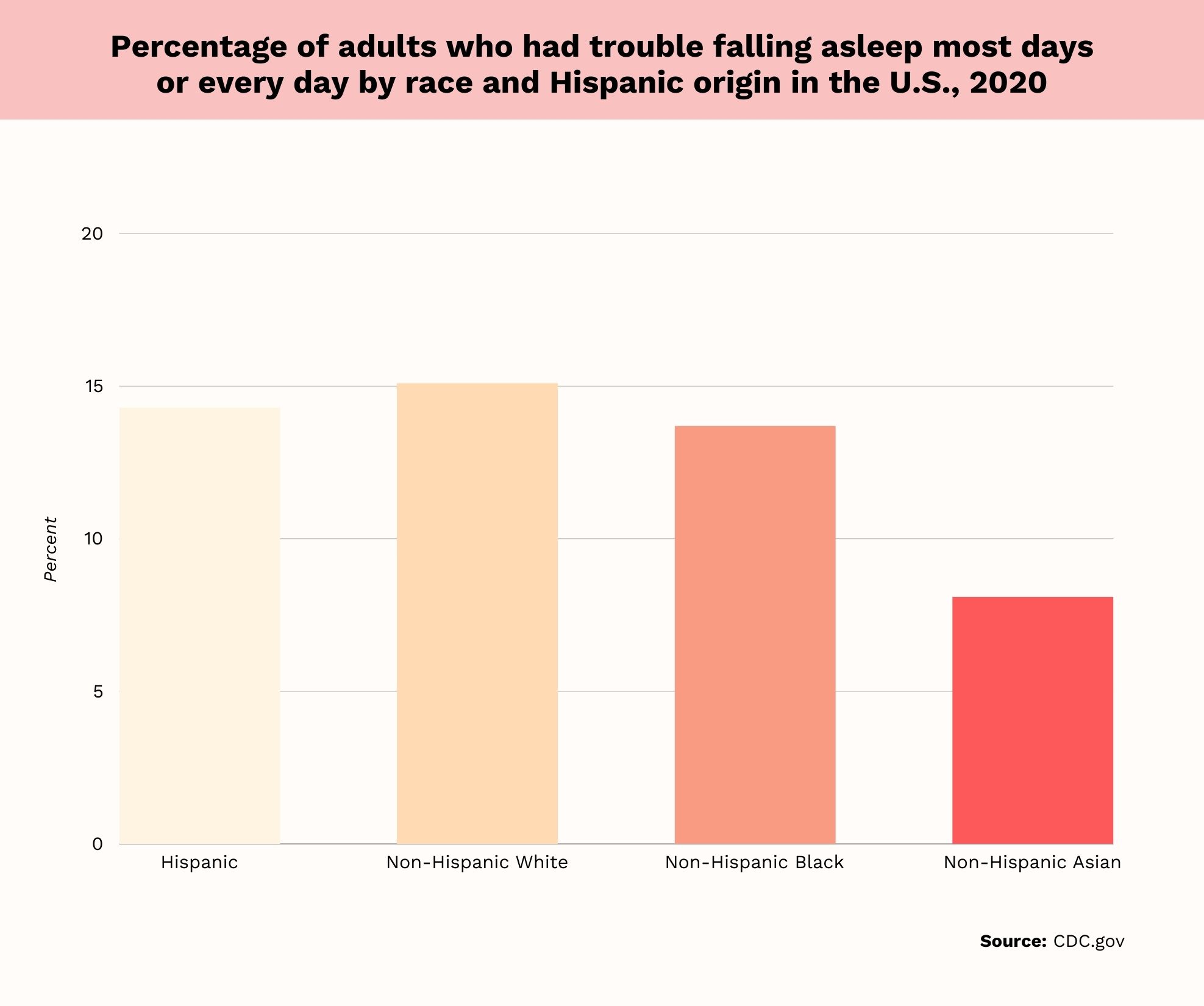
- Among non-Hispanic Whites, 15.1%[2] of people have trouble falling asleep all or most days.
- In Hispanics, 14.3%[2] have difficulty falling asleep all or most days.
- Among Blacks, 13.7%[2] of people have difficulty falling asleep all or most days.
- Finally, 8.1%[2] of Asians have difficulty falling asleep all or most days.
There is variation in the proportion of people who have trouble falling asleep based on race and ethnicity. Non-Hispanic Whites have the highest rates of difficulty falling asleep all or most nights. The rate is lowest among Asians.
Insomnia Statistics By Income
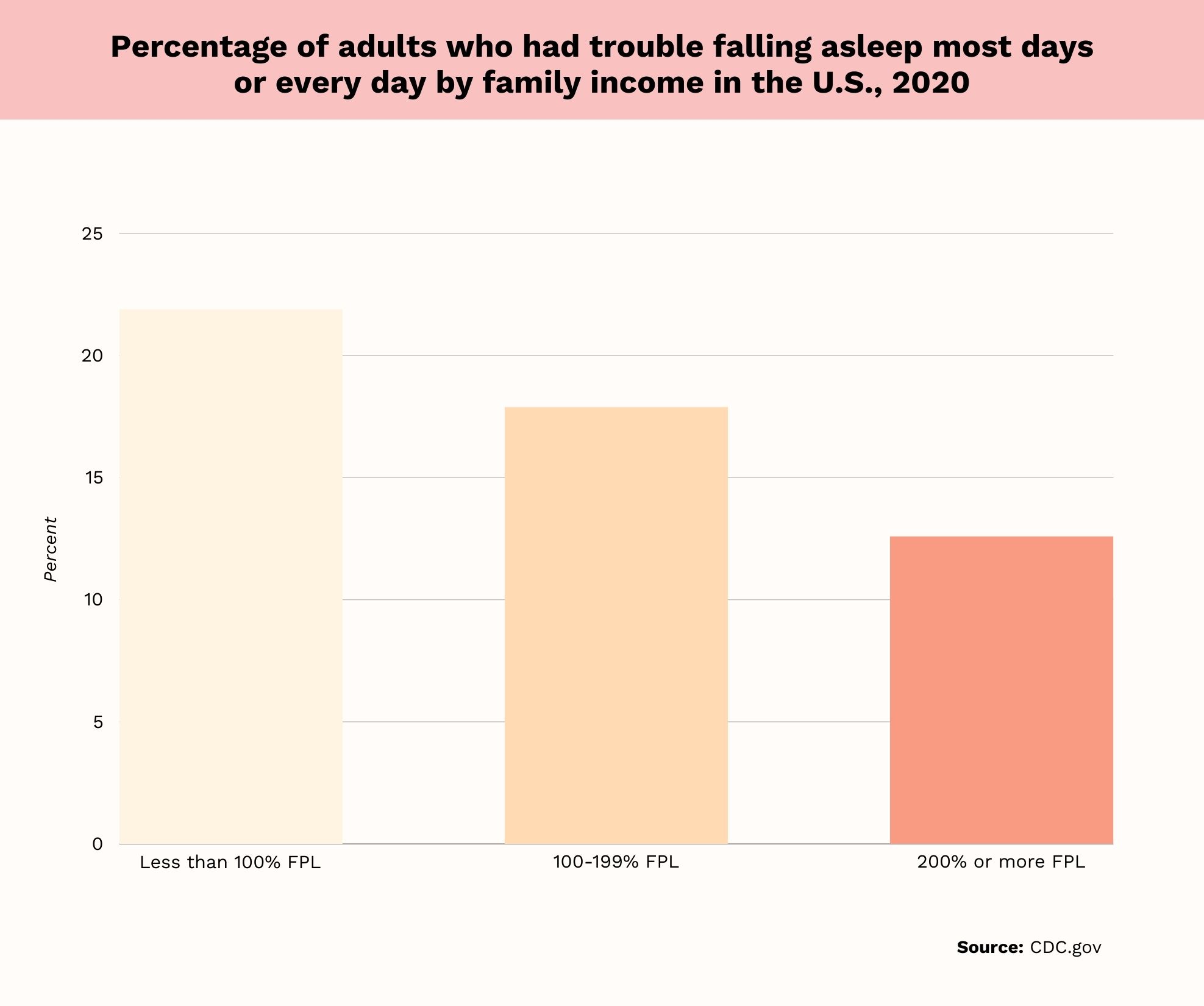
- Among those below 100% of the Federal poverty level, 21.9%[2] have trouble falling asleep all or most days.
- In those at 100%-199% of the Federal poverty level, 17.9%[2] have trouble falling asleep all or most nights.
- In those at 200% of the poverty level or higher, 12.6%[2] have trouble falling asleep all or most nights.
Individuals with higher incomes are less likely to have difficulty falling asleep. The highest rates of difficulty falling asleep are in those below the poverty level.
Insomnia Statistics By Education
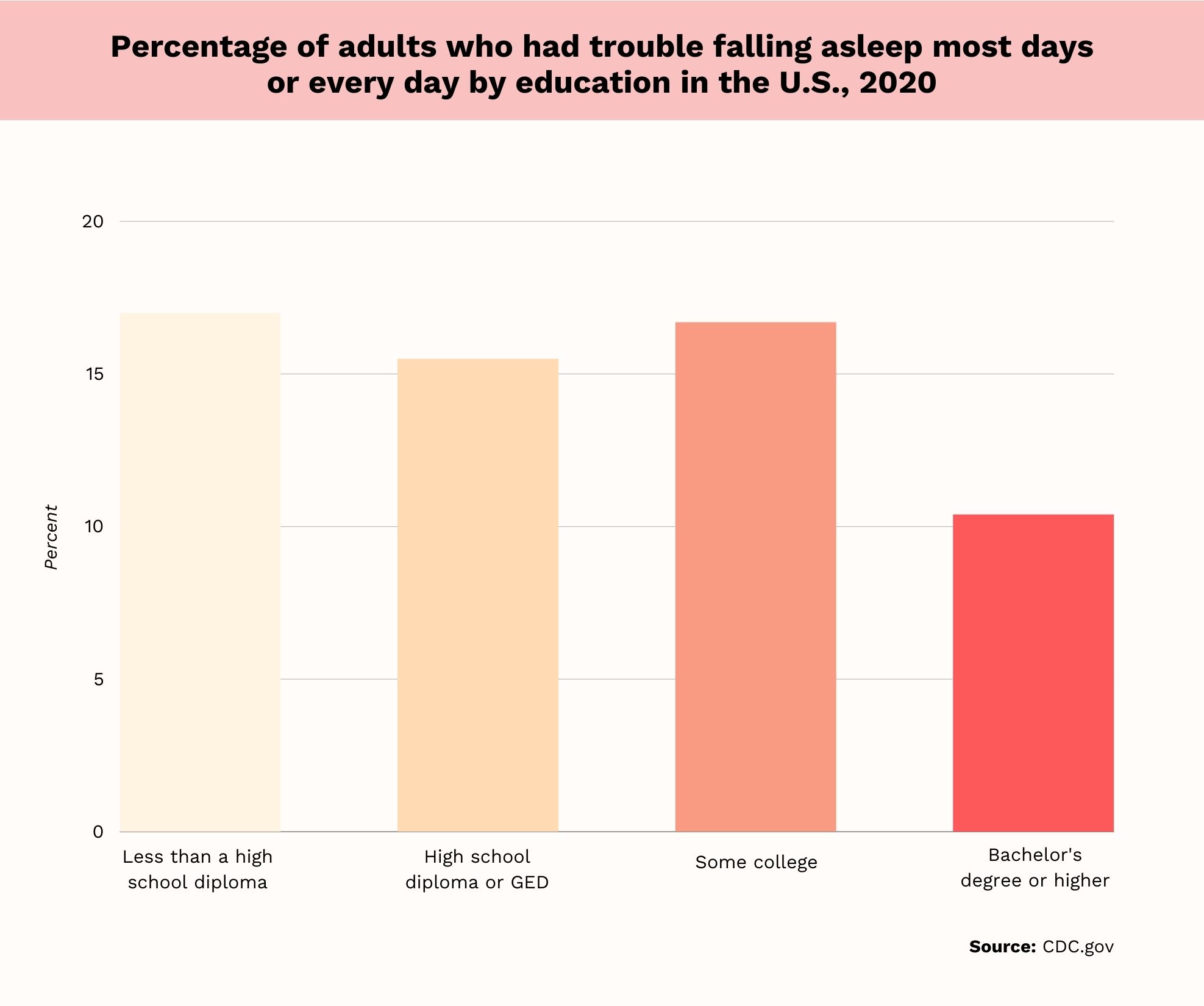
- In those with less than a high school diploma, 17.0%[2] have difficulty falling asleep all or most nights.
- In those with a high school diploma or GED, 15.5%[2] have difficulty falling asleep all or most nights.
- Among those with some college, 16.7%[2] have trouble falling asleep all or most nights.
- In those with a bachelor’s degree or higher, 10.4%[2] have trouble falling asleep all or most nights.
Rates of insomnia tend to decline with increasing education levels. Those with less than a high school diploma will most likely have difficulty falling asleep. People with a bachelor’s degree or higher are least likely to have trouble falling asleep.
Insomnia Statistics By Urbanization Level
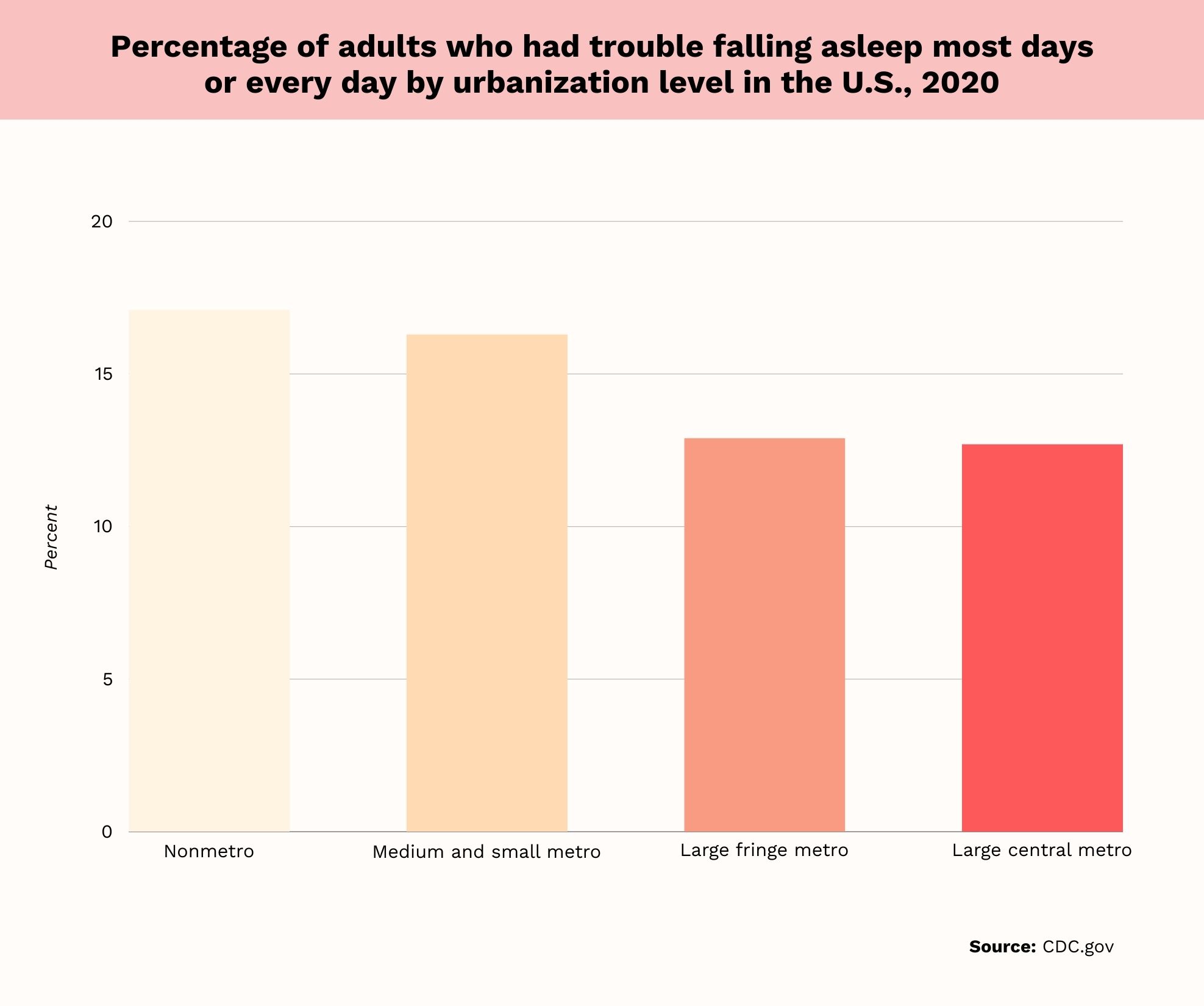
- In non-metro areas, 17.1%[2] of people have trouble falling asleep all or most nights.
- In medium and small metro areas, 16.3%[2] of people have trouble falling asleep all or most nights.
- In large fringe metro areas, 12.9%[2] of people have trouble falling asleep all or most nights.
- In large central metro areas, 12.7%[2] of people have trouble falling asleep all or most nights.
Larger urban areas have lower rates of insomnia than rural locations. The percentage of people who struggle to fall asleep declines in larger cities compared to non-metro areas.
Insomnia Facts To Know
The data above provide information about insomnia prevalence, but there are additional facts to know.
Insomnia Doesn’t Just Involve Trouble Falling Asleep
The data above show the prevalence of people who regularly have trouble falling asleep. However, sleep problem statistics also look at the percentage of people who have trouble staying asleep.
As of 2020, 17.8%[2] of adults had trouble staying asleep all or more nights over the previous 30 days. Of those aged 18 to 44, 13.8%[2] had trouble staying asleep. This is compared to 21.8%[2] of those aged 45 to 64 and 20.3% of those 65 and older.
Insomnia Is Linked To Mental Health
Statistics related to sleep disturbances show a clear link between sleep quality and mental health. Among adults with a mental illness, 50% to 80%[1] struggle to fall or stay asleep over the course of a year. Furthermore, 40%[1] of people with insomnia disorder have at least one psychiatric diagnosis.
In people with insomnia disorder, 23%[1] meet diagnostic criteria for major depression or dysthymia. In addition, 24%[1] experience anxiety, 7%[1] have trouble with alcohol addiction and 4%[1] experience drug addiction.
Short Sleep Duration Is Also Problematic
Having trouble falling or staying asleep, or simply staying up too late, can lead to short sleep duration. For adults, short sleep duration is defined as under 7 hours[3] of sleep per night.
Overall, 32.8%[3] of U.S. adults have short sleep duration. Among men, 33.4%[3] have short sleep duration, compared to 32.2%[3] of women.
The percentage of people reporting short sleep duration varies by age. Below is the breakdown of people with short sleep duration for various age brackets:
Adults aged 25 to 44 have the highest prevalence of short sleep duration. After this age bracket, the prevalence of short sleep duration declines. Those 65 and older have the lowest prevalence of short sleep duration, lower than the 18-24 age bracket.
Insomnia Significantly Affects Quality Of Life
One American insomnia survey found that this condition worsens quality of life. In this study, the percentage of people with insomnia fell to 27.3%.[4] This was the rate for U.S. adults within the previous year.
Study findings also revealed that insomnia results in the loss of 5.6 million[4] quality-adjusted life years annually in the U.S. Insomnia had a more negative impact on quality of life than 18 other medical conditions studied. These included depression, arthritis, and high blood pressure.
Prevalence Of Insomnia Varies Globally
There is a wide global variation in the rate of insomnia symptoms. According to an internet-based survey, the prevalence of insomnia, based on country, was as follows:
- Netherlands: 5.4%.[5]
- Japan: 10.0%.[5]
- Australia: 10.5%.[5]
- United Kingdom: 11.0%.[5]
- United States: 13.4%.[5]
- Germany: 14.6%.[5]
- France: 21.7%.[5]
- South Korea: 23.5%.[5]
- China: 24.0%.[5]
- Brazil: 30.5%.[5]
Based on statistical analysis, insomnia is 2.1 times[5] more likely in France compared to the U.S. In China, it’s 1.77 times[5] more likely, and it’s 2.74 times[5] more likely in Brazil. Finally, insomnia in South Korea is 1.92 times[5] more likely than in the U.S.
Moore states, “Insomnia appears to be increasing in prevalence globally.” She adds, “Factors such as lifestyle changes, increased stress, use of electronic devices before bedtime, and heightened awareness of sleep disorders contribute to its rise.”
Prevalence Of Short Sleep Duration Varies By State
In the United States, there is wide variation in the prevalence of short sleep duration among states. West Virginia has the highest rate of short sleep duration, with 42.8%[3] of adults being short-sleepers. This is closely followed by Alabama, with a rate of 41.2%.[3]
Colorado has the country’s lowest rates of short sleep duration, at 29.3%.[3] Minnesota has the second lowest rate, at 30.1%.[3]
Insomnia Causes And Risk Factors
There isn’t necessarily one single cause of sleep-related disorders like insomnia. Rather, various risk factors increase the chances of a person developing insomnia.
That being said, hyperarousal[6] is considered to be a general cause of insomnia. Hyperarousal refers to a state in which a person is hypervigilant throughout the day. This then leads to difficulty falling asleep and staying asleep at night.
There are two schools of thought related to the effect of hyperarousal. Cognitive models[6] assert that people worry and ruminate, which leads to insomnia. When they cannot sleep, they experience a vicious cycle, as they then worry about lack of sleep.
Other models focus on physiological hyperarousal. According to these models, physiological factors[6] like an elevated heart rate lead to sleep disturbances. An overactive stress system can also lead to higher cortisol levels and disrupted sleep.
According to Dr. Paul Daidone, MD, FASAM, Medical Director at True Self Recovery, “Stress, anxiety, depression, chronic pain, and certain medications are among the leading causes of insomnia.” He states, “Furthermore, lifestyle factors such as poor sleep habits, irregular work schedules, and caffeine and alcohol consumption can all contribute to the development of insomnia.” He concludes, “Sometimes, underlying medical conditions such as sleep apnea or restless legs syndrome can also cause insomnia.”
Insomnia Risk Factors
Several risk factors can interfere with sleep quality and increase the likelihood of insomnia. These risk factors are discussed in more detail below.
Female Gender
Female gender[6] has been identified as a risk factor for insomnia. In the U.S., 17.1%[2] of women, compared to 11.7%[2] of men, have trouble falling asleep.
Furthermore, 20.7%[2] of women, compared to 14.7%[2] of men, have trouble staying asleep.
Having A Mental Health Disorder
Having a mental health diagnosis increases the risk of sleep disorders, including insomnia. Around 40%[6] of people with insomnia disorder have a co-occurring mental health condition. Depression is particularly common in people with insomnia.
In some cases, a mental health condition is a consequence of poor sleep. In other instances, mental illness is a risk factor for insomnia symptoms. In people with depression, common pathologies[6] underlying both depression and insomnia can be at play.
Genetics
In some cases, your genes[7] can increase your risk of insomnia. This condition can run in families, and genes can influence whether you’re a light sleeper.
Poor Sleep Environment
Your sleep environment[7] also plays a role in how well you sleep. A noisy, bright sleep environment can lead to poor sleep quality. Uncomfortable temperatures, whether too high or too low, can also disrupt sleep.
Lack Of Physical Activity
Not getting enough exercise can interfere with your sleep health. One study found that compared to active adults, inactive adults were 22%[8] more likely to develop insomnia.
Shift Work
Shift work can interfere with circadian rhythms and lead to insomnia symptoms. A systematic review of five studies found insomnia prevalence was higher in shift workers[9] than in the general population.
In one of the studies, the prevalence of insomnia in shift workers was as high as 76.4%.[9] In four out of five studies in the review, the insomnia rate exceeded 40%.[9]
Medical Problems
Medical problems can also go hand-in-hand with insomnia. More specifically, diabetes[10] has been found to increase the risk of insomnia.
Patients with obstructive sleep apnea are also more likely to experience sleep disturbance. In one study, 38%[11] of patients with obstructive sleep apnea had insomnia. Among patients, 42%[11] had difficulty maintaining sleep, 18%[11] had difficulty falling asleep, and 21%[11] experienced early morning awakenings.
Substance Abuse
Substance abuse is linked to insomnia.[12] Abuse of drugs and alcohol can lead to sleep disturbances. Substance abuse can also lead to or worsen obstructive sleep apnea, which interferes with sleep.
People may experience sleep problems[12] with chronic substance abuse; intoxication and withdrawal can also lead to sleep disruptions.
Insomnia Treatments
If you have an insomnia disorder, it’s important to take steps to improve your sleep health. A doctor or mental health professional can help you make lifestyle changes to improve sleep. Other insomnia treatments can be divided into behavioral methods, like counseling and pharmacological methods.
Behavioral Treatments For Insomnia
If lifestyle changes do not help, you may be referred to a type of treatment called cognitive-behavioral therapy for insomnia.[13] CBT-I lasts for six to eight weeks, and it’s often the first recommended treatment for chronic insomnia. In CBT-I, you will learn about sleep health and develop strategies to reduce your nervousness about sleep problems.
Moore says, “CBT-I is a highly effective treatment that addresses maladaptive thoughts and behaviors related to sleep.” Dr. Daidone states, “Non-pharmacological treatments include cognitive behavioral therapy, relaxation techniques such as meditation and deep breathing exercises, and improving sleep hygiene.”
Pharmacological Insomnia Treatments
If behavioral treatments are not beneficial, a doctor may prescribe one of these sleep medications to treat insomnia:[13]
- Benzodiazepine receptor agonists: These include zolpidem, zaleplon, and eszopiclone.
- Melatonin receptor agonists: This includes the medication ramelteon.
- Benzodiazepines: Benzodiazepine drugs like triazolam are usually the last choice when other methods don’t work, as they can be habit-forming.
Sleep medications can be beneficial, but it’s important to understand they can cause side effects. Your doctor will work with you to determine whether you need medication to promote sleep health. If your doctor chooses to prescribe medication, it is because they believe the benefits will outweigh the side effects.
Dan Ford, licensed psychologist and clinical director at The Better Sleep Clinic, states, “Sleep medication is considered to be the second line treatment and should be time-limited.” Dr. John says, “The other option for treating insomnia is pharmacological treatment, including over the counter or prescription medications, which I’m not a huge fan of.”
Treatment For Co-Occurring Health Conditions
Finally, if you have symptoms of sleep-disordered breathing, seeking treatment can improve your sleep. Symptoms[14] of obstructive sleep apnea include loud snoring, daytime sleepiness, and gasping for air during sleep. Treatment with a continuous positive airway pressure machine, or C-PAP,[15] can improve sleep and reduce insomnia symptoms.
Tips To Improve Your Sleep Health
If you’re experiencing insomnia, you can improve your sleep health with lifestyle changes.[13] For example, avoiding TV and screens before bed reduces your exposure to bright lights that can disrupt sleep. It’s also important to set a consistent sleep schedule.
Finally, getting regular exercise[13] and avoiding alcohol, nicotine, and caffeine before bed are also helpful. It’s also important to ensure that you’re sleeping in a cool, dark environment.
Dr. John shares, “I encourage people to have a fixed sleep schedule, ideally 10 pm to 6 am, and keep out any light, keep noise to a minimum, and set the temperature low in the bedroom.” He also recommends,”I encourage people to power off their minds and not spend any time worrying in bed.” He states, “Schedule another time to worry, and keep an easy routine.”
Conclusion
Insomnia is relatively prevalent. After all, 14.5%[2] of all U.S. adults had trouble falling asleep on most or all days in 2020. This number can vary based on age, gender, and race/ethnicity, but the bottom line is sleep problems are common.
A variety of risk factors, such as shift work, mental illness, and substance abuse, can cause insomnia. If you’re struggling to sleep, it’s important to make lifestyle changes. You can also reach out to your primary care physician to determine what medical interventions may be beneficial.
Frequently Asked Questions
In 2002, 17.5%[16] of U.S. adults had insomnia or trouble sleeping. This rose to 19.2%[16] by 2012. These rates are comparable to or slightly lower than today’s insomnia rates.[2]
There are several risk factors that make insomnia highly prevalent. For example, having a mental health disorder[6] increases the risk of insomnia. Daily life stressors, which are numerous, can also lead to hyperarousal[6] and sleep problems
 Evidence Based
Evidence Based
