Lupus[1] is a rare autoimmune disorder that involves the immune system attacking healthy tissue. The most common form[1] of lupus is systemic lupus erythematosus. This condition leads to widespread inflammation that can attack multiple tissues and organs.
A person with lupus can experience problems with the joints, lungs, skin, kidneys, brain, heart, and blood vessels. While there is no cure, but lifestyle changes and medical care can improve symptoms.
It is helpful to look at lupus statistics to know who is affected by this autoimmune disease. Learn the top lupus facts below, as well as information about disease management.
Key Lupus Facts
- It is estimated that 1.5 million[2] Americans, and at least 5 million[2] people worldwide, have a form of lupus.
- Systemic lupus accounts for approximately 70%[2] of all cases of lupus.
- Overall, lupus prevalence is at 72.8[3] cases per 100,000 people.
- Compared to White women, Black and Latina women are 1.5 to 3[4] times more likely to develop lupus.
- Over 90%[4] of lupus cases are in women — nine times more likely than men.
- In 2018, 14,263[5] people in the U.S. were diagnosed with systemic lupus erythematosus.
Lupus Statistics
How Common Is Lupus
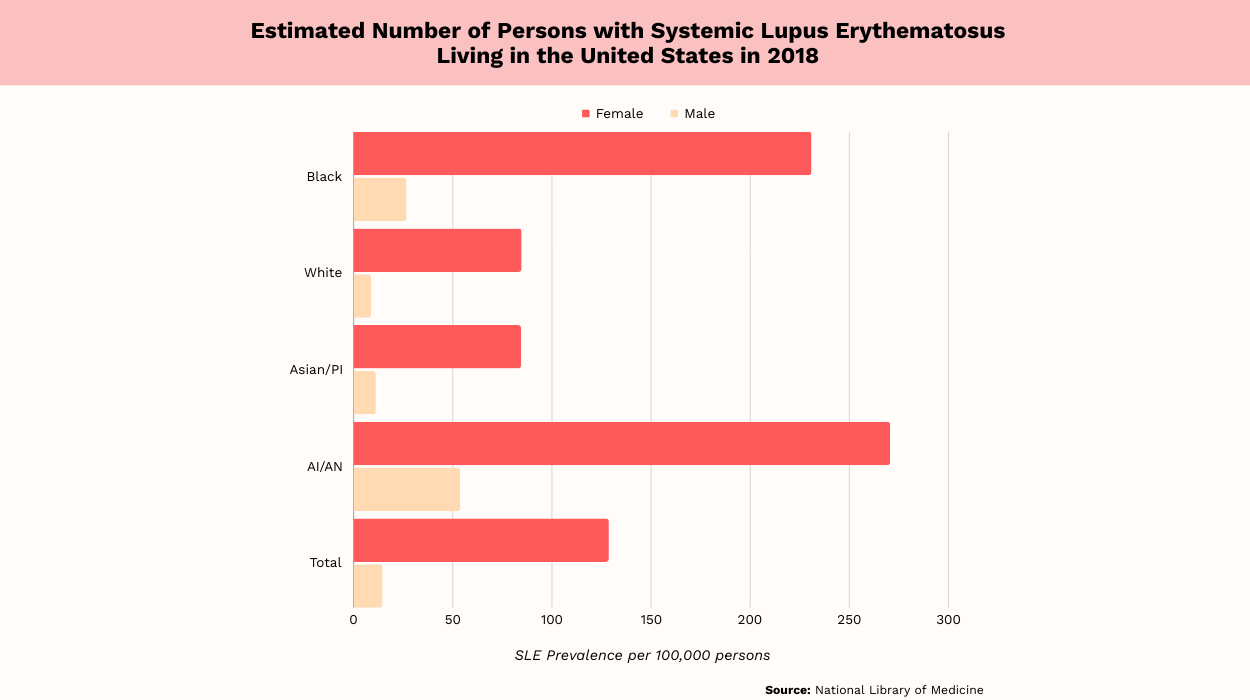
- The overall prevalence of lupus is 72.8[3] per 100,000 people in the U.S. population.
- In men, the prevalence of systemic lupus is 14.6[3] per 100,000, compared to 128.7[3] per 100,000 in women.
- Lupus statistics by race show that the rates are highest in Black women. The prevalence is 230.9[3] per 100,000f for this group.
- For Hispanic women, the prevalence is 120.7[3] per 100,000, compared to 84.7[3] per 100,000 for White women.
- In Asian/Pacific Islander women, lupus prevalence is 84.4[3] per 100,000.
- Among American Indian/Alaskan Native women, the prevalence is 270.6[3] per 100,000.
- In Black men, prevalence is 26.7[3] per 100,000, compared to 18.0[3] per 100,000 for Hispanic men.
- Asian/Pacific Islander men have a prevalence of 11.2[3] per 100,000.
- In White men, lupus prevalence is 8.9[3] per 100,000.
- The prevalence of lupus is 53.8[3] per 100,000 for American Indian/Alaskan Native men.
For all races, the prevalence of lupus is higher[3] in women compared to men — nine times higher. Among all races of women, American Indian/Alaskan Natives have the highest[3] prevalence. American Indian/Alaskan Native men also have the highest[3] lupus prevalence.
New Case Statistics
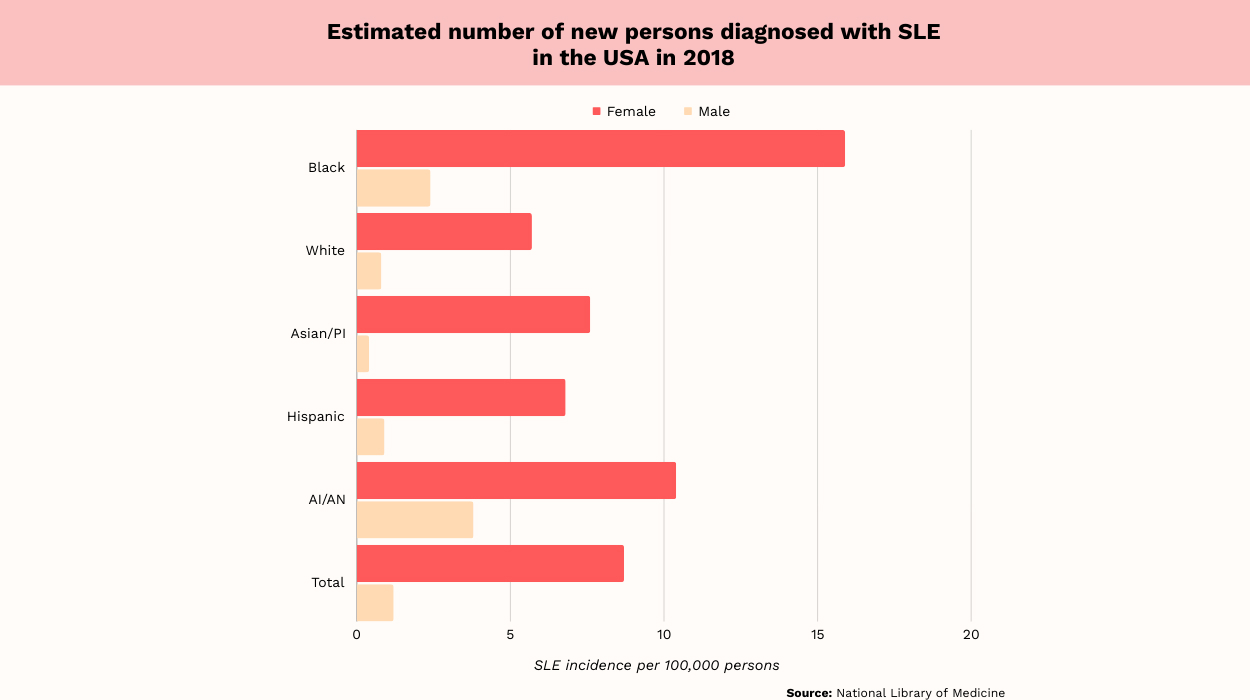
- Overall, the incidence rate of lupus was 5.1[5] new cases per 100,000 people in 2018.
- In women, the incidence was 8.7[5] per 100,000, compared to 1.2[5] per 100,000 for men.
- In Black women, the incidence was 15.9[5] per 100,000, compared to 7.6[5] per 100,000 for Asian/Pacific Islander women.
- Hispanic women had an incidence of 6.8[5] per 100,000, compared to 5.7[5] per 100,000 for White women.
- American Indian/Alaskan Native women had an incidence of 10.4[5] per 100,000.
- Black males had an incidence of 2.4[5] per 100,000, compared to 0.9[5] per 100,000 for Hispanic men.
- White men had a lupus incidence of 0.8[5] per 100,000.
- In Asian/Pacific Islander men, the incidence was 0.4[5] per 100,000.
- American Indian/Alaskan Native men had an incidence of 3.8[5] per 100,000.
Lupus incidence, which refers to new cases of this autoimmune disease, varies based on race. Among women, the incidence is highest[5] among those who are Black. In men, the highest[5] incidence is among American Indians/Alaskan Natives.
According to Dr. Rishabh Nanavati, an orthopedic surgeon, “African Americans, Hispanics, and Asians are disproportionately affected by lupus compared to Caucasians.” Dr. Rishabh further states, “Some genes may increase susceptibility, but their impact varies across ethnicities.”
Lupus Statistics By Age
The incidence of lupus by age for women was as follows, according to the rate per 100,000 person-years in 2002:
- Ages 15-19: 2.6[6]
- Ages 20-24: 3.6[6]
- Ages 25-29: 3.47[6]
- Ages 30-34: 2.56[6]
- Ages 35-39: 1.79[6]
- Ages 40-44: 1.75[6]
- Ages 45-49: 2.58[6]
- Ages 50-54: 2.63[6]
- Ages 55-59: 2.07[6]
- Ages 60-64: 0.91[6]
- Ages 65-69: 1.55[6]
- Ages 70-74: 1.40[6]
- Ages 75-79: 1.30[6]
- Ages 80-84: 0[6]
The incidence rate of lupus by age for men is as follows, according to the rate per 100,000 person-years in 2002:
- Ages 15-19: 0.57[6]
- Ages 20-24: 0.56[6]
- Ages 25-29: 0.46[6]
- Ages 30-34: 0.48[6]
- Ages 35-39: 0.56[6]
- Ages 40-44: 0.58[6]
- Ages 45-49: 0.86[6]
- Ages 50-54: 1.32[6]
- Ages 55-59: 1.40[6]
- Ages 60-64: 1.64[6]
- Ages 65-69: 2.18[6]
- Ages 70-74: 1.45[6]
- Ages 75-79: 1.31[6]
- Ages 80-84: 0.70[6]
The most recent data for lupus incidence by age is from 2016, but it provides a suitable estimate.
Up until the age range of 60-64, women have a higher[6] lupus incidence when compared to men. The incidence for women generally decreases with growing age. By ages 80-84, women’s incidence rate is not greater than zero.
Lupus rates historically are low for younger men and peak in the age range of 65-69[6] years. The lupus incidence rate for women peaks much younger, at 20-24[6] years.
Lupus-Related Death Rate
The risk of death in people who develop lupus can vary based on socioeconomic factors, including race. The five-year survival rate after lupus diagnosis reached about 90%[7] in the 2000s. This was an increase from 1955, when the five-year survival rate in lupus patients was 50%.[7]
The survival rate can vary considerably from the figure above based on race. Standardized mortality ratios show that lupus patients are two to three times[7] more likely to die than the general population.
However, Blacks with a new case of lupus die, on average, at 51.8[7] years old. Whites with a new case of lupus die at an average age of 64.4[7] years. Data from 2017 shows Black women and Black youth with lupus are four to seven times[8] more likely to die than Whites.
Lupus mortality rate disparities between Black and White women vary based on age. Below is the ratio of Black to White lupus deaths based on age category:
These figures mean that Black women and youth are significantly more likely to die from lupus than Whites. In those ages 25-44, Black females are over seven times[8] more likely to die compared to Whites.
According to Dr. Zeeshan Afzal, M.D., “Lupus can range from mild to severe, and while it is typically not fatal, it can lead to complications that may be life-threatening.” Dr. Zeeshan explains, “These complications may include kidney damage, cardiovascular issues, and
infections.”
Lupus Facts To Know
Beyond the general prevalence, incidence, and mortality data above, there are other facts to know about lupus. Consider the information below.
Significant Health Disparities Are Seen In Lupus Patients
Outcomes for lupus patients have improved over time. However, medical advances have not had as much benefit for racial and ethnic minority groups. Compared to White patients, Blacks with lupus have a significantly lower[9] life expectancy.
Low socioeconomic status is a strong contributing factor to health disparities in lupus. Poverty contributes[9] to increased mortality risk from lupus. It is also associated with reduced survival rates[9] in people who develop end-stage renal disease from lupus nephritis. Furthermore, the disorder may be drug-induced systemic lupus erythematosus, or SLE, where such exposure may induce an autoimmune reaction in a genetically susceptible individual.
Finally, ethnic minorities are not well-represented in clinical research that studies lupus treatments. Almost 40%[9] of the U.S. population identifies as a racial or ethnic minority group. However, just 2%-16%[9] of participants identify themselves as being in minority groups in lupus studies, distorting the statistics.
This leads to health disparities because treatment response can vary[9] based on race. Without minority group self-identification, it’s difficult to determine which treatment is appropriate for these groups.
Epidemiological Studies Show Wide Variation In Global Lupus Incidence And Prevalence
Lupus incidence varies widely across the globe. Newly diagnosed SLE has a global incidence of 5.14[10] per 100,000 person-years. This means about 0.40[10] million people are diagnosed each year.
Globally, women have a higher incidence of lupus, at 8.82[10] cases per 100,000 person-years. This is compared to men, who have a global incidence of 1.53[10] per 100,000 person-years.
Incidence estimates are highest[10] in Poland, the United States, and Barbados. Data analysis has also shown that lupus is more common[10] in high-income countries.
Globally, lupus prevalence is 43.7[10] per 100,000 people overall and 78.73[10] per 100,000 women. Prevalence in men is 9.26[10] per 100,000 globally. Disease prevalence is highest[10] in the United Arab Emirates, Barbados, and Brazil.
Lupus Costs Vary By Severity
A U.S. study published in 2021 tabulated annual costs the year before and after a lupus diagnosis was established. Costs varied by the severity of the disease. Patients with mild lupus incurred $13,415[11] in costs the year after diagnosis. The cost was $29,512[11] for moderate lupus and $68,260[11] for severe lupus.
This infers that once the diagnosis is made, those with severe lupus are more aggressively treated than they were before. The primary contributors to these expenses were outpatient visits, which cost $13,566[11] on average annually, and hospitalizations, which cost $10,252.[11]
Economically, the global burden of lupus is quite significant. For instance, in China, the average cost for treating lupus in 2017 was CNY 33,899[12] per patient. This is equivalent to $4,725.39 in the United States.
Studies have shown wide variation in lupus costs across the globe. Countries including the U.S., Canada, the UK, Germany, Greece, Japan, Korea, Hong Kong, and Taiwan have reported costs. Annual cost per patient ranges from $3,735 to $14,410[12] across different countries.
What Is Systemic Lupus Erythematosus — SLE?
Systemic lupus erythematosus is a chronic autoimmune condition. SLE[13] is the most common type of lupus, and it occurs when a person’s immune system attacks healthy tissues, similar to other autoimmune diseases. SLE causes inflammation throughout the body, and it can lead to damage in multiple organs.
When people have SLE, they experience multiple lupus symptoms, which can include:[13]
- Painful joints.
- Extreme fatigue.
- Skin rashes.
- Fever.
- Swollen joints.
- Sensitivity to sun.
- Oral ulcers.
- Psychosis.
SLP can also lead to complications,[13] such as arthritis, lung problems, heart issues, seizures, and kidney disease. Symptoms typically disappear completely when the disease goes into remission,[14] either spontaneously or due to treatment.
Lupus can affect any major organ, but the kidneys are particularly susceptible to damage from lupus. Among patients with lupus, 50%[15] experience kidney problems. Lupus patients are at risk of a type of kidney disease called lupus nephritis.[16]
Types Of Lupus
There are four different types of lupus. SLE, described above, is the most common type. Other types include:[17]
- Cutaneous Lupus Erythematosus: Some people with CLE also have SLE, but others don’t. CLE affects the skin and causes rashes, hair loss, sensitivity to the sun, ulcers, and swelling in blood vessels.
- Drug-Induced Lupus: Certain medications can cause drug-induced lupus, which is similar to SLE in symptom profile. People with drug-induced lupus experience joint and muscle pain and fever. Drug-induced lupus is usually caused by medications that treat seizures, high blood pressure, and rheumatoid arthritis.
- Neonatal Lupus: Neonatal lupus is a rare disease impacting infants who receive antibodies from their mothers who have lupus. Infants with neonatal lupus present with skin rash, liver problems, and low counts of blood cells. The condition typically goes away on its own but can lead to serious heart defects.
Living With Lupus
Lupus is a chronic disease, and there is no cure. However, you can learn to manage symptoms through lifestyle changes and medical treatment. These are described in more detail below.
Lifestyle Changes For Lupus
A healthy lifestyle is particularly important if you live with lupus. If you smoke, it’s important to give it up to reduce[18] disease activity. Getting some physical activity and following a healthy diet are also[18] important.
Exercise may alleviate[18] fatigue and improve quality of life. A diet high in polyunsaturated fatty acids[18] is also beneficial and can reduce disease activity. You can add these healthy fats[19] to your diet by consuming fish, flaxseed, or supplements.
Medical Treatment For Lupus
The goals of lupus disease management are to reduce flares, alleviate symptoms, and prevent organ damage. Lupus is primarily treated with the following medications:[20]
- Nonsteroidal anti-inflammatory drugs — NSAIDs — which include over-the-counter medications like ibuprofen.
- Corticosteroids like prednisone.
- Antimalarial drugs like hydroxychloroquine and chloroquine phosphate.
- BLyS-specific inhibitors, most commonly belimumab.
- Immunosuppressive agents or chemotherapy, are only used when other treatments fail.
- Specific medications to treat conditions like high blood pressure.
Beyond taking medication, some people may need to see a specialist, such as a nephrologist, if they have kidney damage.
Conclusion
Among all the autoimmune diseases, lupus is quite rare, affecting 72.8[3] per 100,000 people in the U.S. However, lupus disproportionately affects certain groups, including[5] Black women. Women[6] of childbearing age are also more likely to experience lupus.
Given the economic costs, health disparities, and complications associated with lupus, it’s important to raise awareness. Ongoing research should focus on disease management strategies, especially for women of color.
Frequently Asked Questions
Lupus[13] is a chronic autoimmune disease that causes symptoms like joint pain, extreme fatigue, and skin rashes. The most common type of lupus is systemic lupus erythematosus.
Lupus is a moderately rare disease, affecting just 72.8[3] per 100,000 people in the United States.
Lupus can lead to death, and lupus patients have a higher[7] mortality rate. Common causes of death[20] include[20] infection, kidney disease, and cardiovascular disease. However, you can live a long life with proper lupus treatment.
The exact cause of lupus is unknown. It is believed to be caused[13] by hormonal, environmental, and genetic factors. Black women[5] and those of childbearing age[6] are at increased risk of lupus compared to other groups.
 Evidence Based
Evidence Based