Leukemia[1] is a group of blood cell cancers that advance at different speeds. These types affect specific age groups, with some types more common[2] in children and others more common in adults Leukemia is the tenth most common cancer in the U.S.
This bone marrow disorder causes an influx release of blood cells. The result is the creation of abnormal blood cells that crowd out the healthy cells.
An experimental hematology and oncology article[3] states that the most common types are
- Acute lymphoblastic leukemia, or ALL. This is common in children 2 to 5 years old and young adults.
- Acute myeloid leukemia, or AML, is prevalent in adults, accounting for 1.3% of cancer[3] cases in America.
- Chronic lymphocytic leukemia, CLL, is common among older adults.
- Chronic myeloid leukemia, CML, is common among older adults.
Other blood cancers are myeloma, myeloproliferative neoplasms, and myelodysplastic syndromes. The myelodysplastic syndrome occurs when blood cells are inadequately formed or don’t work right.
Here we’ll highlight leukemia statistics and facts.
Key Leukemia Facts
- Blood cancer statistics predict that about 59,610[4] people will be diagnosed with leukemia in 2023.
- About 437,337[4] people in the U.S. are living with or are in remission from leukemia.
- Statistics estimate that approximately 23,710[5] deaths in America will be attributed to leukemia in 2023.
- Leukemia cancer types make up 3.0%[4] of all new cancer cases in America.
Leukemia Statistics In The United States
Leukemia has two main types: Acute and chronic. Here are the main differences between acute and chronic leukemia.
- Progression: Acute leukemias progress faster within a few weeks or months. Chronic types take longer than a few months.
- Cells that are attacked: Acute leukemias affect immature blood cells that grow to malfunction. Chronic types affect mature blood cells; they may still function but not at their best.
- Treatment: Acute blood cancers require aggressive treatments like chemotherapy, radiation, or bone marrow transplant. Chronic blood cancers are less aggressive with treatments like targeted drugs, chemotherapy, or immunotherapy.
A 2020 paper on the prevalence of leukemia globally[3] highlights the following:
- Between 1990 and 2017, there was a decreasing number of leukemia incidences.
- Acute myeloid leukemia and chronic lymphocytic leukemia types increased between 1990-2017.
- The incidence rates of leukemia across different regions are heterogeneous. This means new cases differ across different groups based on other factors.
Some factors that may lead to new high leukemia cases in America are as follows. These affect both the leukemia survival rate in a child and the leukemia survival rate in adults.
- The vast population compared to other smaller locations globally.
- Other possible factors are environmental, access to healthcare and genetic predispositions.
You can boost the survival rates by proper disease management. Dr. Sridhar PS, from Clinicspot, had the following to add on how to do that
“For individuals with chronic leukemia, the focus is on managing the disease over an extended period. This includes:
Regular monitoring helps track the disease and identify any changes requiring further treatment. Taking medication as prescribed: Medication adherence is crucial for controlling the disease and preventing complications.
Adopting healthy lifestyle habits:
* Eating a healthy diet.
* Exercising regularly.
* Getting enough sleep can help improve overall health and well-being.”
Who Gets Leukemia?
Leukemia may affect anyone and at any age. Still, here is the breakdown of who gets it:
- Age: It affects all ages. Approximately 3,000 children get a leukemia diagnosis[6] in the U.S. yearly. A 2018 paper highlights that adults in the U.S. have a 1.5% lifetime[7] risk of developing all types of leukemia.
- Gender: Men are more likely to get diagnosed with leukemia than women. A recent study highlights that the total number of deaths per population[8] in men in North America was 21.7/100,000. The women’s death rate was 15.1/100,000. Mortality rates are up to 40% higher in males, possibly related to higher smoking rates and occupational hazards.
- Race: Asian and Pacific Islanders have a lower diagnosis. Whites have the highest[9] percentage of cancer history, especially for CML.
- Other risk factors: Family history,[10] genetic mutations,[11] chemical and medical exposure,[12] smoking,[13] Down syndrome,[14] and lower awareness[15] and diagnosis prevalence.
Leukemia Statistics By Age
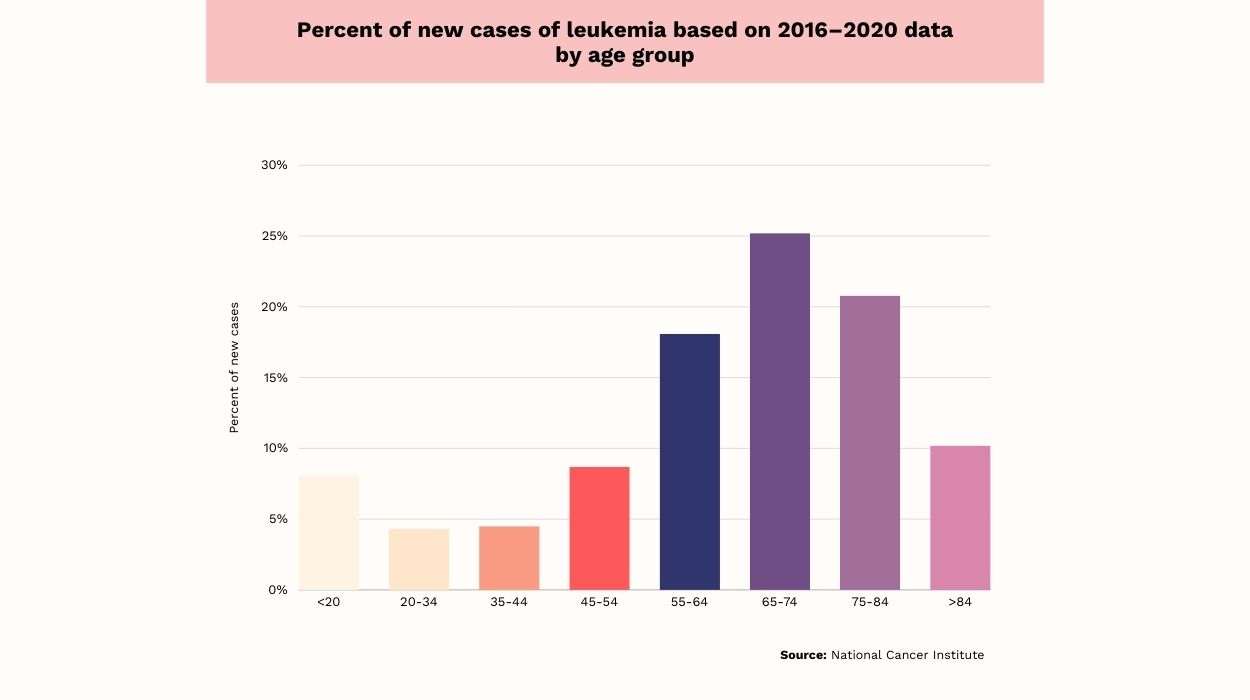
Here is the breakdown of the above chart of leukemia statistics based on age[4] between 2016 and 2020 for new cases diagnosed:
- Adults between 20-34 and 35-44 present the lowest new leukemia cases. Each is approximately 4.5%.
- The age group 65-74 marked the highest percent of new cases at 25%, followed by the 75-84 group with 21%, then the 55-64 age group with 18%.
- Adults between 45 and 54 marked approximately 9%.
- Older adults above 84 comprise about 10%.
- The estimated number percentage was about 8% for children and adolescents younger than 20.
Leukemia Statistics By Race/Ethnicity & Sex

Here are the leukemia statistics based on race or ethnicity[4] per 100,000 persons for 2016-2020:
- In all races, males had higher rates of leukemia at 17.8/100,000.
- Non-Hispanic whites had the highest numbers at 19.6/100,000.
- The second race is non-Hispanic Asian or Pacific Islanders at 16/100,000.
- Non-Hispanic American Indian or Alaskan native men recorded the lowest prevalence. The rate was at 15.9/100,000 persons.
- There was a small difference between Hispanic and non-Hispanic blacks. Both are approximately 13.2/100,000 and 13.7/100,000, respectively.
In general, females marked an 11/100,000 person rate of new cases.
- Non-Hispanic whites rates ranked highest at 11.7/100,000.
- Non-Hispanic American Indian or Alaskan native females ranked second with about 10.1/100,000 persons.
- The Hispanic and non-Hispanic black women tied at the rate of 9.2/100,000 persons each.
- Non-Hispanic Asian or Pacific Islander women recorded the lowest numbers at 6.5/100,000 persons.
Leukemia Death Rate
Leukemia cancer death may occur for many reasons, but infections are prevalent.
- In children’s acute lymphoblastic leukemia cancer group, of the 74 kids, 43.2% died of infections.[16]
- In another study on 313 patients, 84 died due to infections. Of these patients, 67% of the deaths[17] were due to lung infections.
Besides infections, here are other causes of leukemia fatalities:
- Bone marrow failure[18] due to significant hemorrhage or bleeding.
- Pneumonia.[19]
- Lack of medical intervention.
Percent Of Deaths By Age Group
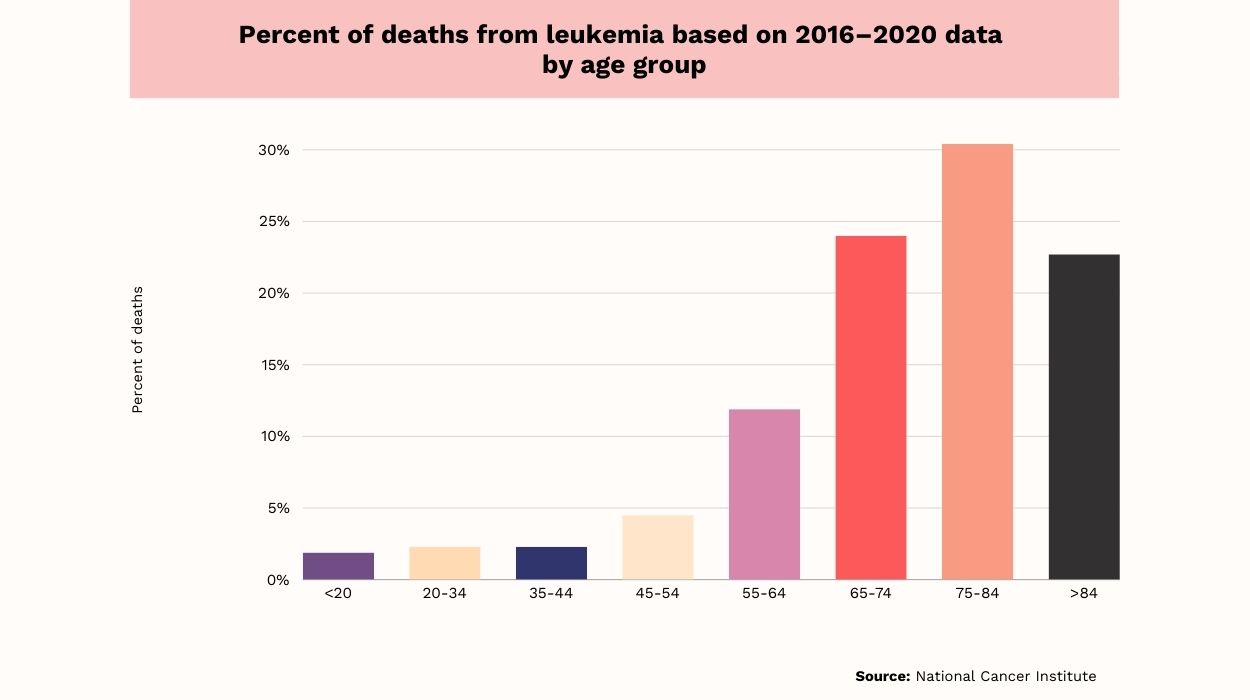
Here is what the above age-adjusted death rates chart represents:[4]
Generally, the older age groups had a higher death percentage.
- Individuals aged 75-84 had the highest mortality data at 30.4%.
- The 65-74 at 24% and groups over 84 at 22.7% were second and third.
- The 55-64 age group was fourth at 11.9%.
- The age group 45-54 was fifth in mortality at 4.5%.
- The groups 20-34 and 35-44 were among the lowest at 2.3%.
- The death percentage of children and young adults under 20 was lowest at 1.9%.
Death Rate By Race/Ethnicity & Sex

In all races, men record the highest death toll at 8/100,000 persons.
- Non-Hispanic whites recorded high deaths at 8.6/100,000 persons.
- Non-Hispanic black men recorded about 6.8/100,000 deaths.
- Non-Hispanic American Indian or Alaskan native men’s death toll comes third at 5.8 per 100,000 persons.
- Non-Hispanic Asians 4.5% and Hispanic men 5.4% recorded the lowest death percentages.
Women had a lower death rate at 4.5/100,000 persons compared to men.
- Non-Hispanic white women recorded the highest death toll at 4.7/1000,000 persons.
- Non-Hispanic black women register the second highest rates at 4.3/100,000 persons.
- The lowest rates of cancer deaths are Hispanic, non-Hispanic American Indians, and non-Hispanic Asians. The data is 3.5/100,000, 3.2/100,000, and 2.5/100,000, respectively.
Leukemia Survival Rate
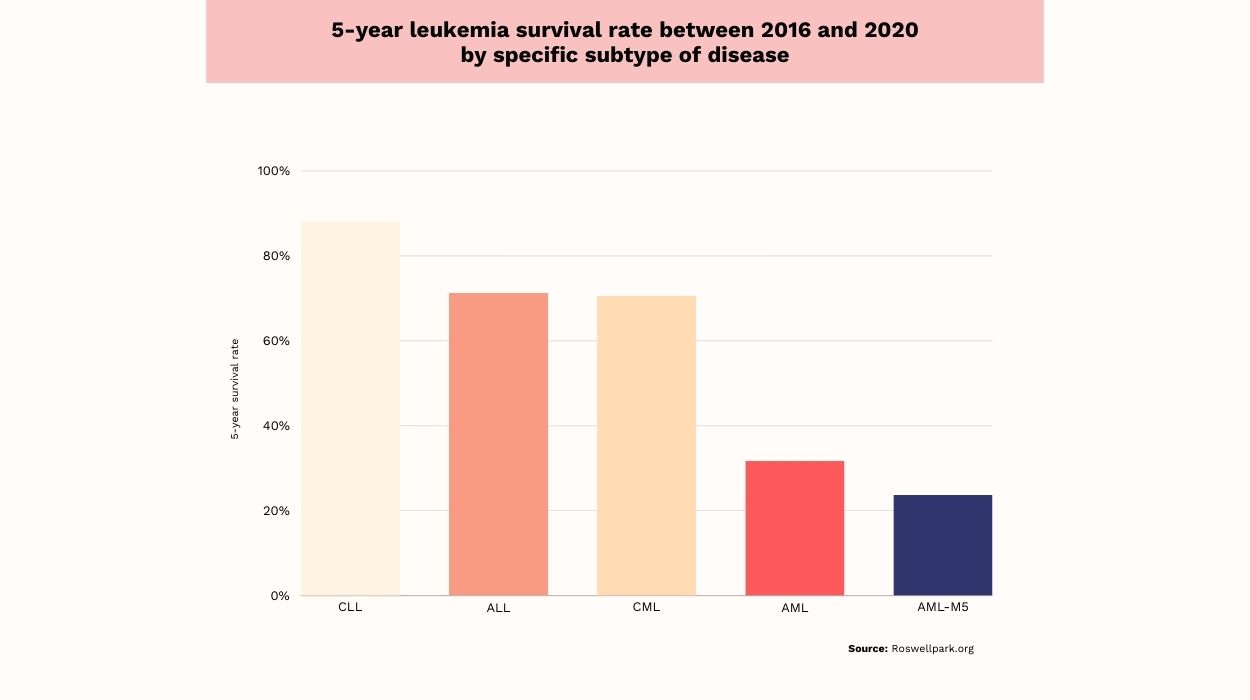
In the United States, the 5-year survival among people diagnosed with leukemia is 65%. Yet, these statistics differ according to the specific leukemia subtype:
- Chronic lymphocytic leukemia’s five-year relative survival rate is 88%.[20]
- Acute lymphocytic leukemia’s 5-year relative survival rate is 71.3%.[20]
- Chronic myeloid leukemia, or CML’s 5-year survival rate is 70.6%.[20]
- Acute myeloid leukemia’s survival rate in 5 years is 31.7%.[20]
- Acute monocytic leukemia’s survival rate in 5 years is 23.7%.[20]
Leukemia Facts To Know
Leukemia Affects All Age Groups
This blood cell cancer affects people of all ages. According to leukemia age statistics, it is highest in adults over 74 years and lowest in the age group 20 to 34. It also affects children younger than 15.
Leukemia Affects More Men Than Women
Men are more predisposed to developing and dying from leukemia[8] than women. According to one report, they attribute the gender disparities to the following possible risk factors.
- Smoking and occupational carcinogens.
- Women have estrogen with some protective effects.
- Genetics.
- Immunity.
In Some Cases, External Factors May Cause Leukemia
Radiation, chemical contamination, or smoking exposure may cause the development of leukemia. Other possible factors under investigation are
- Exposure to electromagnetic fields,[21] pesticides and herbicides,[22] and air pollution.[23]
Symptoms Of Leukemia
Leukemia manifests through the following symptoms:[24]
- Tiredness and weakness.
- Weakened immune system and recurrent infections.
- Reduced red blood cell count, causing paleness.
- Easy bruising and impaired blood clotting.
- Enlarged lymph nodes.
- Loss of appetite and weight loss.
- Excessive sleep sweating.
- Breathlessness because of reduced red blood cells.
Some of these symptoms are common to other health issues. So, to be sure it’s leukemia, consult a doctor for diagnosis and treatment.
And since diagnosis can be stressful, here is what Dr. Zeeshan Afzal, with a background in clinical science and the subject, suggests:
“– Seek Support: Join support groups, talk to friends and family, and consider individual counseling to address emotional needs.
– Education: Understanding the disease and treatment options can help alleviate anxiety and empower patients to make informed decisions.
– Lifestyle: Maintain a healthy lifestyle with a balanced diet, regular exercise, and adequate sleep to improve overall well-being.
– Mindfulness and Relaxation: Techniques like meditation, yoga, and deep breathing can help reduce stress and anxiety.
– Professional Help: Consider consulting a mental health professional for therapy or counseling if needed.”
How Is Leukemia Diagnosed?
Here is what a leukemia diagnosis[25] comprises:
- Blood Tests: Doctors carry out blood tests to diagnose the condition.
- Bone Marrow Aspiration: Doctors extract a small bone marrow sample and examine abnormal cells.
- Bone Marrow Biopsy: A biopsy offers a more extensive view of the bone marrow structure beyond aspiration. This helps doctors establish the disease staging and understanding of cell morphology.
- Cytogenetic Analysis:[26] This analysis helps doctors uncover how a patient’s leukemic cells will react to therapy.
- Immunophenotyping:[27] This routine diagnostic work-up helps classify leukemic cells.
- Lumbar Puncture:[28] This is a cerebrospinal fluid test for leukemia cell infiltration.
- Imaging Studies: For further scrutiny, healthcare professionals use X-rays, CT scans, or MRIs. These help identify any enlarged lymph nodes.
- Genetic Testing:[29] This is usually helpful if there is a family history of leukemia. Gene testing highlights genetic mutations that may influence disease progression and treatment response.
- Flow Cytometry:[30] This test quantifies cell characteristics, aiding leukemia subtype classification.
- PCR or Polymerase Chain Reaction:[31] This amplifies and analyzes DNA to detect genetic abnormalities associated with specific leukemia types.
Diagnosing leukemia early helps healthcare professionals offer better-targeted treatment strategies.
This is what Dr. Sridhar PS, from ClinicsSpot, had to say about the recent medical advancements that improved long-term survival rates:
“Recent medical advancements have significantly improved long-term survival rates for people with leukemia. These advancements include:
Targeted therapies: These drugs target specific mutations in leukemia cells, leading to more effective treatment with fewer side effects.
Immunotherapies: These therapies harness the body’s immune system to fight cancer cells. Stem cell transplantation: This procedure can replace diseased bone marrow with healthy stem cells, potentially curing the disease. Improved supportive care: Advances in supportive care, such as better infection prevention and management, have also improved survival rates.”
Leukemia Treatments
Doctors customize leukemia treatment since all cases are unique. Nonetheless, here are the available leukemia treatments:
- Chemotherapy entails the administration of powerful drugs to eliminate multiplying leukemic cells. Using blinatumomab with chemotherapy in infants with acute lymphoblastic leukemia has a two-year survival rate of 81.6%.[32]
- Targeted[33] therapy is a precise way of delivering medication by targeting abnormalities in leukemia cells. This minimizes healthy cell damage.
- Immunotherapy[34] boosts your immune system to destroy leukemia cells. This is the best for patients not eligible for intensive chemotherapy.
- Stem Cell Transplantation[35] replaces damaged bone marrow with healthy stem cells. This transplant encourages normal blood cell production.
- Biological Therapy[36] is the administration of living organism substances that change the body’s response to leukemia.
- Combination Therapies use several treatments at the same time for better effectiveness.
- Tyrosine Kinase Inhibitors,[37] i.e., TKIs, target specific leukemia cell growth enzymes. It’s a common approach in certain leukemia types like the CML.
- Hormone Therapy[38] involves regulating hormone levels to control leukemia cell growth.
- Intrathecal Therapy is the administration of medications directly into the cerebrospinal fluid. These prevent or treat central nervous system involvement. As per research, many doctors use these three medications:[39] Methotrexate, cytarabine, and hydrocortisone.
You should be diligent with treatment to increase the leukemia recovery rate. Early intervention boosts the leukemia cure rate for curable types like acute lymphoblastic leukemia.
Dr Bart, a Harvard and Johns Hopkins-trained plastic surgeon, said the following about getting personalized treatment plans.
“Personalized treatment plans are crucial for improving the outcomes for leukemia patients. These plans are based on the individual patient’s unique characteristics, such as the type of leukemia they have, their age, their overall health, and their genetic make-up. This allows for a more tailored approach to treatment, which can be more effective and have fewer side effects.
A study published in the journal Blood found that patients with acute myeloid leukemia (AML) who received personalized treatment plans had a significantly higher survival rate than those who did not. This study highlights the importance of personalized medicine in improving outcomes for leukemia patients.”
Conclusion
All the above facts and statistics on leukemia highlight that it can affect all ages and genders. However, it’s more common in men than women for a few reasons. One popular reason is the exposure to occupational carcinogens.
Still, early diagnosis is the best remedy to manage the condition better. Doctors may suggest several therapies, including hormonal, intrathecal, biological, and chemotherapy. They offer these or other remedies after diagnostic testing, such as blood tests, bone marrow aspiration, or biopsy.
And if you have any queries on this blood disorder, they answer questions with accurate information.
Because leukemia has a few subsets, treatments and management routines vary. Some might respond better to chemo while another biological therapy. Whatever the case, please stick to the recommended treatment and stay committed.
Continuous research and care will enhance survival rates and reduce these cancer statistics. It’ll also improve the quality of life of those affected by leukemia while lowering the mortality figures.
Frequently Asked Questions
Yes, you can, thanks to the advanced treatments, early detection, and personalized care. Regular medical follow-ups and adherence to treatment plans enhance life expectancy.
Leukemia is a severe and life-threatening condition. Its severity depends on factors like type, stage, and individual response to treatment.
Acute myeloid leukemia AML is often considered more aggressive, leading to rapid progression. Outcomes vary, and therapy advancements continue to improve prognosis.
While you may manage many cases of chronic leukemia, some forms, like chronic myeloid leukemia, aren’t curable. However, ongoing research and evolving treatments offer hope for improved long-term outcomes.
Leukemia patients and their families can access various support services. These include counseling, support groups, and educational resources.
 Evidence Based
Evidence Based
